May 21, 2018
May 2018 Newsletter

Carlos A. Pellegrini, MD, FACS Chief Medical Officer, UW Medicine and Vice President for Medical Affairs
Welcome to the new online Care Transformation newsletter on our revamped Care Transformation website. This site will be home for helpful information on care transformation efforts, where you can read newsletters, view videos, access resources and get background on key strategies. We recently introduced two ongoing education campaigns – our “Road to Care Transformation” video series and “The Transformer: the UW Medicine Care Transformation Podcast.” We hope you’ll find these materials engaging and informative as you learn more about the work being done by your colleagues – like this month’s C-Section Pathway and Hypertension updates – to advance our delivery of high-value care. If you have feedback, want to share best practices, suggestions for newsletter updates, project spotlights, video stories or podcast topics, etc., please e-mail us at uwmedway@uw.edu. Thanks for all you do for UW Medicine to help us fulfill our mission of improving the health of the public.
C-Section Pathway Reduces Postpartum Complications

Whether planned or unplanned, a Cesarean section is a stressful event for families and clinical teams. In an effort to optimize patient experience and reduce postpartum complications, a team at UW Medical Center (UWMC), led by Jane Hitti MD MPH and Emily Fay MD, developed a standardized pathway for C-section care.
The “UW Medicine Way” for C-section focuses on prenatal patient education, an ambulatory protocol, evidence-based practices for intraoperative and postop management, and minimized opioid use. “There was consensus across patients, educators, physicians, nurses, and in-patient/out-patient care teams,” said Hitti. “They were all pleased to have a standard work pathway that’s patient-focused and based on best practices.”
Culture change was key and nurses were pivotal to the success of the pathway. Fay developed a patient care map, now translated into four languages. Nurses review the care map and an educational PowerPoint with the patient before her C-section. These materials are also available online and on the recently launched UW Baby app.
“Explaining the pathway’s benefits and setting expectations empowers patients and families to follow along, understand the process and also seems to speed up recovery,” added Hitti.
The pathway is used for both planned procedures as well as postpartum for unanticipated C-sections. As a result of lots of hard work, at present, UWMC has one of the lowest CS rates in the state amongst our Boeing- and PEBB-contracted populations (generally, mothers with no chronic health conditions).
The C-Section pathway has been getting lots of use and has achieved substantial results. From implementation in April 2017 through March 2018, there have been 593 patients on the pathway (72% of all eligible patients). Postpartum length of stay has gone down by 17% (a reduction of half a day) for planned C-sections and 13% for both planned and unplanned, with total costs dropping approximately 12%. There was also a significant decrease in readmissions — cut almost in half on unplanned procedures.
The C-section pathway will soon be expanded to Valley Medical Center and Northwest Hospital.
Pathway Credits: Maternal-Fetal Medicine: Jane Hitti, MD MPH; Emily Fay, MD; Anesthesiology: Laurent Bollag, MD; Carlos Delgado Upegui, MD; Labor & Delivery: JoAnn Slater, RN; Micah Bailey, RN; Internal Consultant: Blair Mills
Second BP Reading Improves Hypertension Control
Did you know that May is National High Blood Pressure Education Month? This national campaign, part of the Stroke Awareness campaign of the CDC in partnership with the American Heart Association, aims to make all people aware of their blood pressure, and all people with high blood pressure more aware of what they can do to control it and reduce their risk of stroke and heart disease. Controlling high blood pressure and hypertension is a major focus at UW Medicine and practitioners have an EPIC tool at their disposal to help discuss lifestyle management and high blood pressure education with their patients. They can easily enter the smartphrase “.BPLIFESTYLE” in the patient’s electronic medical record and review and print out key information and action steps.
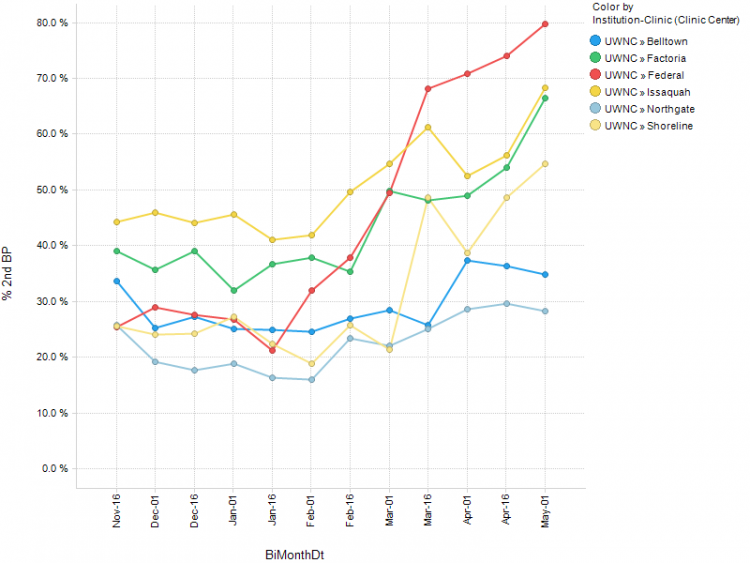
Using this smartphrase is just one component of the Hypertension Pathway, led by D.C. Dugdale MD and Pam Yung MD, launched at six of our Neighborhood Clinics in mid-March. Another technique helping us make significant improvements in blood pressure control is taking a second BP measurement during the same visit if the first is 140/90 or greater.
“Our goal in BP measurement is to make it as accurate as possible and research has shown that if a first reading is high, when you take a second reading, the accuracy of the whole measurement process improves,” said Dugdale. “Our pilot has shown that 25-35% of the time, the second reading has resulted in controlled levels — thereby avoiding excessive treatment.”
The new BP measurement process created by the pathway has already paid off with substantial increases in the pilot clinics from their baseline in December. With a 50% goal for April, four clinics achieved this mark with Federal Way hitting it out of the park at 80%. The four-month goal of the pilot is to reach 80%.
Briefly (Kudos & Credits)
- UW Medicine was recently honored by the Centers for Medicare & Medicaid Services (CMS) for success with one of our Transforming Clinical Practice initiative (TCPi) Patient and Family Engagement milestones – Patient Activation. Details of our Patient Activation Measure (PAM) pilot were presented at the 2018 CMS Quality Conference. Our story was one of three awarded out of 80+ submissions. The pilot was noted for its dedication to patient engagement and for our use of the PAM tool, a 10-13 question survey which assesses a patient’s knowledge, skill, and commitment to self-management of their care by generating an activation score. Key improvements from the pilot, which is supported by care management teams from across the UWM system, include updated disease monitoring readings, a decrease in uncontrolled chronic conditions (diabetes, hypertension and depression), as well as significant improvements in mean PAM scores.

Population Health Management centralized Care Management Team (l-r) Medical Director Elizabeth Paesch, Program Managers Erica Strait and Nkem Akinsoto, Director of Patient Outreach & Care Management Tammy Wilson, with the CMS award.