Care Transformation
Strategies & Tactics
Strategy:
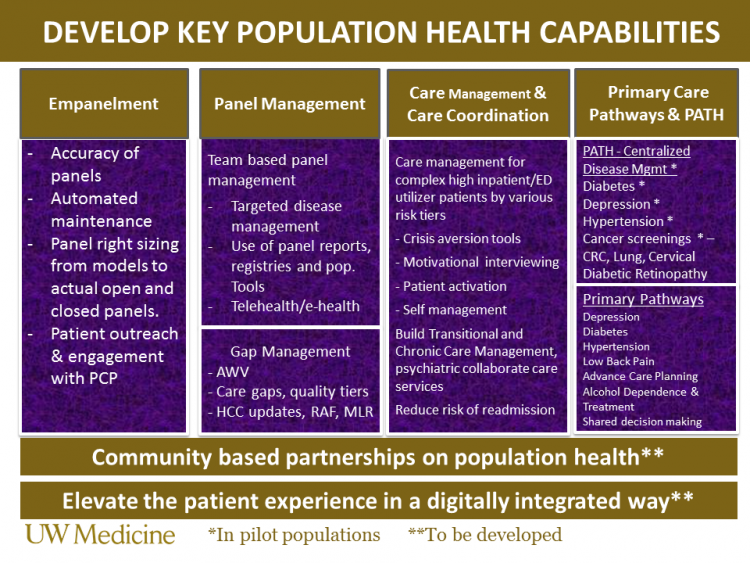
Develop the “UW Medicine Way” of caring for our populations by broadening our focus beyond “sickness” to “wellness” care and establishing services to prevent disease, promote health and reduce the burden of chronic illnesses.
2018 Tactics:
- Continue to develop appropriate panel maintenance tools for primary care provider (PCP) teams to assess panel status and maintain accurate panels.
- Education around who changes the General PCP field and how to use the care team functionality
- Maintenance of accurate panels for empaneled providers
- Develop and deploy a UW Medicine empanelment policy
- Ensuring active engagement and contact to patients on panels who haven’t seen their PCP recently (at 30, 34, 36 months)
- Monitoring the un-empaneled patient population and developing workflows to assign and manage appropriately for health outcomes.
- Furnish proactive panel management and health maintenance on patients empaneled to a UW Medicine primary care provider (PCP).
- Ensure PCP teams have the right tools to forecast, deliver care so patients stay current on their annual wellness checks, preventative screenings and immunizations throughout the year and manage better controlled status for patients coping with chronic diseases (e.g. Depression, Diabetes, Hypertension)
- Scale AWV and care gap outreach to other eligible patients and grow new revenues.
- Leverage team-based task delegation to facilitate clinical care team efficiency and satisfaction.
- Grow new revenue opportunities and improve quality metrics towards targets in our value-based contracts through robust gap management programs (e.g. Boeing, PEBB, Premera AHS, Medicare Advantage, Regence AHN, TCC, Premera GOC)
- Furnish Annual Wellness Visits (AWV), close care gaps and HCC gaps for Medicare Advantage and expand to other eligible populations like Medicare traditional.
- Focus on furnishing transitional care management (TCM) for populations vs. hospital patients – with central PHM and Post-Acute Care support.
- Give patients the extra help they need through care management, better care transitions and coordination of care.
- Develop and operationalize a care transitions strategy that is proactive and connects back patients traversing the continuum of different health settings to their PCP team. Reduce readmission risk and unnecessary inpatient and emergency department visits.
- Provide self-management tools so patients are better equipped to personal health crisis episodes
- Provide chronic care management (CCM) to eligible and identified patients.
- Develop evidence based ambulatory protocols and outlier management surveillance methods to better manage patients with chronic diseases or outreach to patients with disparities on achieving better health maintenance
- PCPs partner with Population Health Management (PHM) PATH programs to close outlier and preventative screening gaps (e.g. furnish FIT test or colonoscopies, A1c, PHQ9, BP, lung cancer screening)
- Develop and implement three primary care pathways to better manage chronic disease:
- Depression
- Hypertension
- Diabetes