
PEARLS is an effective skill-building program that helps older adults manage and reduce their feelings of depression and isolation. Some older adults might also describe those feelings as chronic sadness, loneliness, frustration, being overwhelmed, or losing interest in things they love.
PEARLS adapts to the participant and the place and the need. The program is used by numerous cultures and communities. By removing barriers related to race, poverty, and where someone lives, PEARLS makes mental health services more available to underserved communities. Sessions with older adults take place in their homes or other community-based settings that are more accessible and comfortable for older adults.
PEARLS is simple and easy to administer by staff at community-based organizations who might not have previous counseling experience or a higher education. There is PEARLS training that prepares staff to provide the program to community members.
PEARLS Coaches

PEARLS coaches are the heart and soul of an organization’s PEARLS. They are the staff at community-based organizations who meet one-on-one with older adults to help them build the skills they need to live happier, healthier, and more independent lives. PEARLS coaches are a participant’s support, cheerleader, and connection to resources.
This close partnership between a PEARLS participant and coach builds throughout the six to eight one-hour PEARLS sessions. These sessions occur over the course of four to five months, starting with weekly sessions and tapering to monthly. This is a common skill-building technique used to support people in gradually learning to problem solve on their own.
We provide training to become a PEARLS coach, as well as ongoing support for coaches.
PEARLS Reach
National
12,838+ older adults
211 organizations
35 states + D.C.
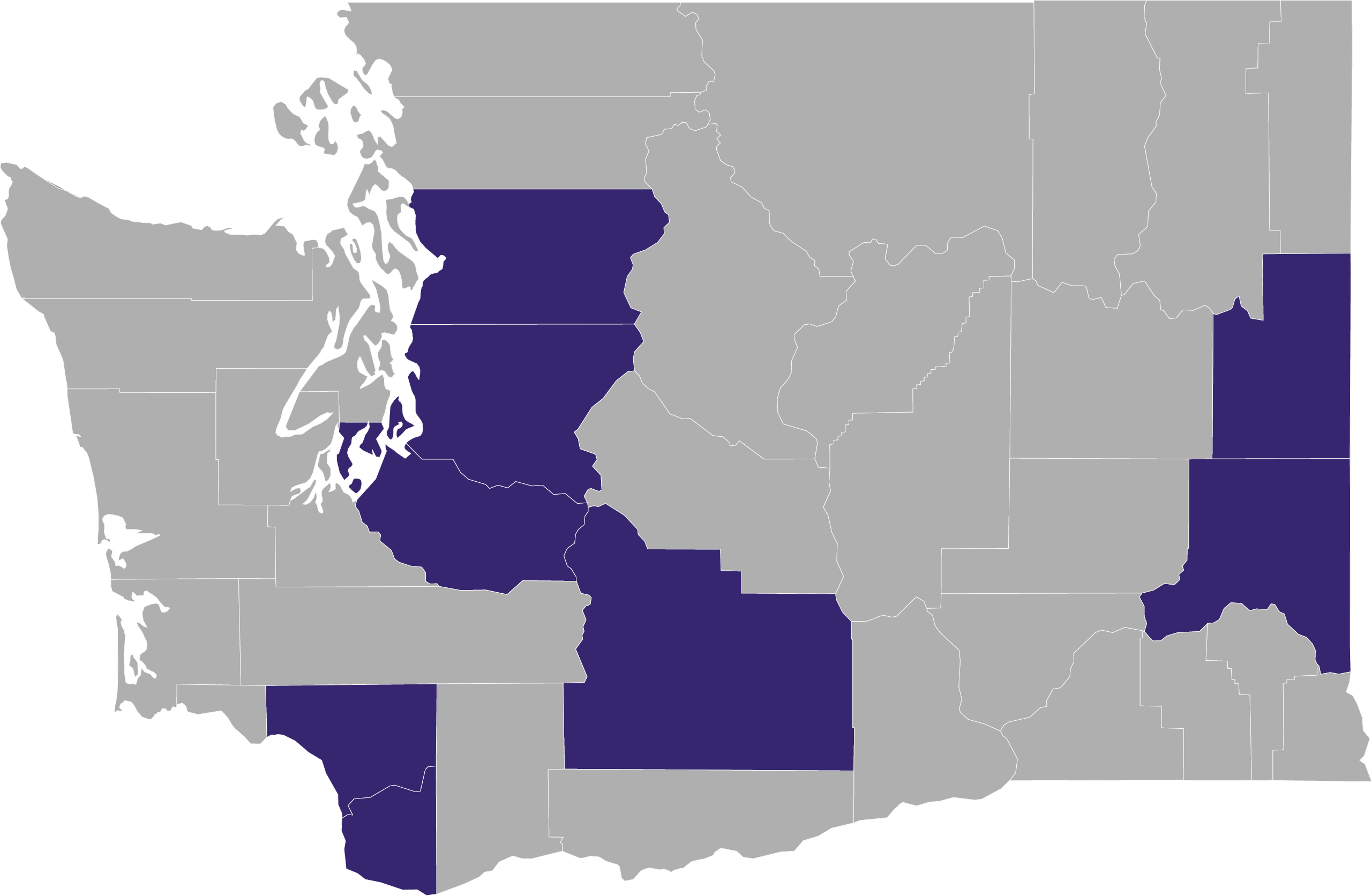
Washington State
2,150+ older adults
17 organizations
8 counties
Our Partnerships
Partnerships with community-based organizations and organizations that providing funding for programs such as PEARLS are what make this program possible.
Here is what a few of our partners had to say about our collaborative efforts with PEARLS.
“I see the UW Health Promotion Research Center as our personal cheerleaders. They celebrate our accomplishments with us and help us troubleshoot when we are struggling.”
Amelia, El Sol Neighborhood Educational Center
(San Bernardino, California)
“With the UW Health Promotion Research Center, we feel more confident. They enable us and empower us to continue our linkages with older folks and our veterans.”
Sluggo, Filipino Senior & Family Services
(Seattle, Washington)
“The UW Health Promotion Research Center partnership provides accessible, non-judgmental support and expertise. They engage and brainstorm with us on ways to reduce barriers to offerings in our rural communities.”
Susan, Rogue Valley Council of Governments Senior & Disability Services
(Central Point, Oregon)
“I really appreciate the UW Health Promotion Research Center’s understanding and flexibility when my clients have their own unique challenges and needs. The UW partnership and programs have been very effective among people with different cultural and linguistic backgrounds, including in our community.”
Syed, Union for Pan Asian Communities
(San Diego, California)
Frequently Asked Questions (FAQs)
Learn more about the Program to Encourage Active, Rewarding Lives or PEARLS™ and how it works. We have divided questions into four categories, although some questions and responses may overlap.
- Overview of PEARLS™: These are questions regarding the nature of PEARLS™ – who it serves, its impact, and research that supports the program.
- Getting Started with the Program to Encourage Active, Rewarding Lives in your Community: These are questions related to what’s required to create PEARLS™ in your community (e.g. staffing, funding, and resources).
- Providing PEARLS™ in Your Community: These are questions about promoting or sharing PEARLS™ coordination and operations.
- Spreading the Word About PEARLS™: These are questions about recruiting participants, promoting the program, and sharing PEARLS™ information with their community.
Please note: We refer to staff at community-based organizations who provide PEARLS™ to older adults as PEARLS™ coaches (formerly referred to as ‘counselors’). Organizations can choose to use the term coaches or can adapt this term for what works best for their community.
Overview of PEARLS
These are questions regarding the nature of PEARLS™ – who it serves, its impact, and research that supports the program.
What is PEARLS?
PEARLS™ is an evidence-based program that helps older adults with depression create happier, healthier lives. The program educates older community members about what depression is (and is not) and helps them develop the skills they need for self-sufficiency and more active lives. PEARLS™ offers a home or community-based setting that is more accessible and comfortable for older adults who do not see clinical mental health programs as a good fit for them, while also allowing for coordination with their current health care providers.
PEARLS™ is simple and easy to administer by staff at community-based organizations who might not have previous counseling experience or higher education. There is PEARLS™ training that prepares staff to provide the program to community members.
PEARLS™ coaches (the name we give frontline staff at community-based organizations providing the program) meet one-on-one with older adults for six to eight one-hour sessions, typically over the course of four to five months. The program begins with weekly sessions that gradually taper to monthly. This is a common skill-building technique used to support people in learning to problem solve on their own.
The University of Washington PEARLS™ team provides long-standing and deeply rooted support, including establishing PEARLS™ as an evidence-based program. The UW Health Promotion Research Center (HPRC) supported PEARLS™ from its early development, and is committed to its success. We offer several training opportunities through the year. Those who complete training are eligible to participate in free, ongoing support – participation in monthly technical assistance calls with us and networking with other organizations that provide PEARLS™ around the country.
How is PEARLS different from other depression programs?
PEARLS is one of only a handful of programs that focuses on helping older adults develop the skills they need to maintain their health, happiness, and independence. The program is part of a cultural shift in how depression is managed by and for aging community members. Most programs address depression in older adults using only the clinical mental health toolkit (counseling and/or medication).
PEARLS™ teaches people skills to actively manage overwhelming problems that contribute to their depression, focusing on the here and now. The participant drives the program – selecting what problems they would like to address, defining reasonable goals, identifying possible solutions and weighing the pros and cons of each solution, and coming up with a feasible action plan. PEARLS™ was designed to be delivered at home, or in another place accessible for the participant. Some people do PEARLS™ and then engage in other traditional therapies, or do PEARLS™ in addition to other programs.
PEARLS™ was designed in collaboration with the organizations that deliver it, validated in partnership with the communities who use it, and adaptable to the people who need it. Support offered through the program is tailored to the individual needs of older adults.
Who can participate in PEARLS™?
PEARLS™ serves all older adults, especially those who have limited access to depression care because of systemic racism, trauma, language barriers, low income, and/or where they live. Older adults do not need be diagnosed with depression in order to participate in PEARLS™. Organizations screen potential participants for depressive symptoms using tools we provide. It is most important that the older adult is able to make decisions and be involved in the PEARLS™ process. Participants need to be able and willing to engage.
Because PEARLS™ was designed in collaboration with the organizations that deliver it and validated in partnership with the communities who use it, the program address various community needs and helps expands access to depression care in underserved communities, including rural ones.
Organizations have provided PEARLS™ to older adults who also receive other mental health or addiction services, and with participants who are on medication. Additional therapies and services should be provided outside PEARLS™ sessions and with a staff member or partnering organization that is not the participant’s PEARLS™ coach.
Which communities have had success with and been positively impacted by PEARLS™?
Through ongoing PEARLS™ research and ongoing assistance activities, we have learned PEARLS™ can positively impact unique populations and address health situations. Below are some of these communities. View a full list of communities or groups that have participated in PEARLS™.
- Military Veterans & Their Partners: Aging and Disability Services in King County, Washington has had much success using PEARLS™ to support veterans and their partners. Recruitment and mental health stigma may be a barrier, but we encourage building a strong rapport with your local veteran community and its members.
- Racial & Ethnic Communities: PEARLS™ has been successfully served agencies that focus on specific racial and/or ethnic populations. Having a PEARLS™ coach from the same or similar cultural background as a participant is helpful but not required. If this is possible, having a community representative who can build a bridge between the coach and the participant is another option, as is providing cultural humility and cultural competency training for staff.
- LGBTQIA Community Members: The LGBTQIA community has benefited from PEARLS™, especially those who may be isolated and face stigma as a LGBTQIA community member. They may also be experiencing the loss of a partner and no adult children, which can add to their isolation, loneliness and/or depression.
- Rural Communities: These communities tend to have fewer transportation options and can be more isolated, including limited access to internet. Meeting older adults in their homes can be a huge advantage of PEARLS™. In rural areas, the coach provides connection to additional community services that might be difficult for isolated older adults to access. We recommend some sessions occur in the home or a community setting, especially the first two sessions. It is also possible to provide PEARLS™ sessions over-the-phone or online.
- Low-Literacy: A PEARLS™ coach can read worksheets aloud and may have a caregiver help an older adult fill out worksheets, as long as the caregivers or coach does not make decisions on behalf of the PEARLS™ participant.
- Mild Cognitive Impairment: If a participant is still able to focus during the session and complete goals, you may be able to include them in PEARLS™. Participants can engage caregivers to assist with activities; however, it is essential the caregiver not do the activity for the participant.
- Mental Illness: PEARLS™ has been benefited those with bipolar or other mental illnesses if they are managing their condition and/or on medication. Participants should be able to focus during sessions and complete goals.
- Substance Use: PEARLS™ has benefited those with substance use disorder if they are managing their condition so they are able to focus during the session and complete goals.
For what client age is PEARLS™ most effective? Are there age restrictions?
We have no age restrictions on PEARLS™ (early studies indicate that PEARLS™ can be effective for adults 18+, not just older adults). Consult your funder. We work with organizations who define older adult differently – 50+, 55+, 60+, 65+, etc., and all these older adults see success with PEARLS™.
The PEARLS™ program could be used for the 18–50-year-old age range. We’ve found that the program has been effective in a separate study on 18-year-olds with epilepsy and have anecdotal evidence from organizations currently doing PEARLS™ with different age ranges. We don’t have programs that cater to a younger demographic. A resource you may take a look at is the National Institutes of Health Database of evidence-based programs.
Can PEARLS™ serve participants who speak languages other than English?
Yes. There are organizations that offer PEARLS™ in languages other than English.
We have translated many of our PEARLS™ materials into other languages, including Chinese (Mandarin), Farsi, Korean, Russian, Somali, Spanish, and Vietnamese. We also recommend reviewing translated materials with native speakers from the community to ensure that the language is appropriate
The PHQ-9 – the questionnaire used to measure individual progress during PEARLS™ sessions) is offered in more than 80 languages.
Contact us for copies and links to translated materials.
Which organizations have had success with PEARLS™?
Organizations with the most successful programs are ones where PEARLS™ aligns with their organization’s mission. Successful programs are those delivered by staff at community-based organizations who can visit older adults in their homes or in community settings that are outside of traditional mental health settings. PEARLS™ has also been implemented at community mental health agencies and has been successful at organizations that support underserved communities. For more info visit our website.
More than 9,400 older adults and 133 organizations across 26 states have participated in PEARLS™. See what some of our partners have to say about our work together.
We also maintain a database of PEARLS™ programs across the country. For a specific list by state and/or city contact us.
How do I know if PEARLS is a good fit for my organization?
To answer, ask, “Does PEARLS align with my organization’s mission?”
If your organization’s mission includes these factors, PEARLS™ could support your efforts:
- Improving health (including behavioral health)
- Focusing on the most common issues that older people face
- Empowering participants to direct their own recovery by teaching them self-management skills
What are some benefits and challenges to seeing older adults in their homes (the PEARLS™ model)?
There are benefits and challenges to seeing older adults in their homes. Knowing both the benefits and challenges will help your organization decide if the program is a good fit. Knowing the potential challenges to visiting people in their homes will also allow you to brainstorm and consider solutions.
Benefits
- Participants are served in a place where they are comfortable and feel more in control
- Participants don’t have to go anywhere (minimized barriers to accessing services)
- No stigma of going to a therapist’s office
- Participants connect to the outside world via the PEARLS™ coach
- Allows you to see the participant in their home environment and get a more holistic picture (e.g. photos of their grandchildren, bare cupboards, fall risks, possible hoarding); this can also help you better understand what existing supports they have available
Challenges
- Travel time required by a coach, which can limit the number of people they see in a day
- Some participants might be reluctant to have someone enter their home (e.g., people with hoarding issues or family members who feel threatened by the older adult working on issues with someone like a PEARLS™ coach)
- Some home settings are unsafe or difficult to visit (e.g., homes with pest infestations, cigarette smoke, strong odors, etc.)
In challenging situations related to home visits, meeting in community settings where you can have privacy and the participant feels comfortable or meeting virtually or by phone can be other options.
Can PEARLS be done with current clients or do we need to recruit new ones?
You do not necessarily have to recruit new clients to provide PEARLS™. Your agency may already be reaching more isolated community members or those experiencing depression (a clinical diagnosis is not needed). PEARLS™ can help your organization expand or enhance current services you already provide.
With PEARLS™, communities have the tools to recognize and respond to depression as an illness that can be treated and managed. Many community-based organizations describe high levels of depression and social isolation among the older adults they serve. This should not be accepted as a normal part of aging.
If your organization is not already serving people who can benefit from PEARLS, you will need to partner with organizations that support underserved older adults, such as Meals on Wheels, senior service agencies, or visiting nurse associations.
We can provide more details and support for recruitment as needed. You can also find information about marketing materials in the FAQs section for “Spreading the Word About PEARLS.”
Where can I find information about the research behind PEARLS™?
We have conducted two RCTs with PEARLS™ to demonstrate significant improvement in depressive symptoms – the first was the original PEARLS™ efficacy trial with older adults, the second RCT was with all-age adults living with both depression and epilepsy (6-and-12-month findings and 18-month findings) one month after PEARLS™ participation ended.
We’ve also recently looked at other outcomes like social connectedness (multi-site single group mixed methods evaluation) and health services utilization (quasi-experimental study looking at inpatient hospitalization and nursing home stays); however, these did not use RCT study design.
There have been several studies conducted to date to better understand how PEARLS™ is being implemented. These studies include a study to examine implementation barriers, which resulted in a pilot study with medically trained interpreters with Russian- and Somali-speaking older adults and an examination of facilitators and barriers to reaching underserved communities, and a study to develop and assess a self-report fidelity instrument.
You can find information about the research studies behind PEARLS™, including research specific to isolation and depression, on our website. If you need additional resources or information, please feel free to contact us.
Within the context of PEARLS research studies, how do I know this program will work for the population we serve?
The two PEARLS™ randomized controlled trials included frail, homebound elders with 4 – 5 multiple chronic conditions and all-age adults with co-occurring epilepsy. For both studies, the majority of participants were low income. 25% in the epilepsy study and 42% in the study with older adults identified as a racial/ethnic minority. In a later study of underserved elder populations and through our work providing technical assistance to PEARLS™ providers, we learned that PEARLS™ has been successful with other populations, such as veterans and vet spouses/widows, immigrants and refugees, elders with limited mobility, and elders in rural settings. Read more about different populations.
To be clear, PEARLS™ did not work for everyone in the original RCTs and may not work for all of your participants. For example, in the first PEARLS™ RCT with older adults, only half of PEARLS™ participants experienced a significant response (50% of more reduction between their pre- and post PHQ-9).
How has PEARLS™ been recognized in national evidence-based registries?
See the agencies and organizations that have recognized PEARLS™ as an evidence-based program. The list includes but is not limited to:
- Administration for Community Living (ACL)
- Agency for Healthcare Research and Quality (AHRQ)
- Archstone Foundation
- Centers for Disease Control and Prevention (CDC)
- engAGED: The National Resource Center for Engaging Older Adults
- Evidence-Based Leadership Collaborative (EBLC)
- Guide to Community Preventative Services (The Community Guide)
- National Registry of Evidence-based Programs and Practices (NREPP)
- Osteoarthritis Action Alliance (OAAA)
- SANHSA’s National Registry for Effective Programs and Practices (NREPP)
In addition, PEARLS™ received the 2011 Archstone Award for Excellence in Program Innovation.
What can you share regarding Return on Investment (ROI) for PEARLS™?
Below are several PEARLS™-specific examples and recommended methods from the EBP field. Please contact us with any questions.
Potential cost savings through decreased health services utilization
Steinman, 2023. Can a Home-Based Collaborative Care Model Reduce Health Services Utilization for Older Medicaid Beneficiaries Living with Depression and Co-occurring Chronic Conditions? A Quasi-experimental Study.
This paper reports on a study we did where we found that PEARLS™ participants compared to similar Home and Community-Based Services (HCBS) participants had lower inpatient hospitalizations and nursing home stays. We used Medicaid claims data to evaluate these reductions in health service utilization. While we did not have costs of services available, these costly health service utilizations are often used as proxies for ROI.
This Playbook 2024 blog Coaching Older Adults to Manage Depression: Program to Encourage Active, Rewarding Lives from the Center for Health Care Strategies describes this article + possible ROI from two PEARLS™ programs (Maintaining Active Citizens in Maryland and El Sol in California).
Zivin, 2013 The economic, public health, and caregiver burden of late-life depression. This paper describes the indirect and direct costs of late-life depression; we focused on health services utilization given this is such a large driver of the burden of depression.
Self-Reported Health Services Utilization: This 4-item self-report measure asks about Outpatient Visits to PCPs, Visits to Emergency Departments, Number of Hospitalizations, and Nights in Hospital as these utilizations are all associated with costs. This measure is built into Well Ware and is available to any PEARLS™ programs to measure pre/post PEARLS™ (and at follow-up after the program ends) if you would like to track costs. Ritter, 2001 article Self-reports of health care utilization compared to provider records provides evidence on this brief measure being comparable to patient records.
Tracking costs of PEARLS™ delivery
We used the methods described in this article to track costs of PEARLS™ delivery for a case study we did in partnership with the AIMS Center and El Sol.
Any ROI study needs to measure costs of implementation so this method can help do this over an intensive one-month data collection period rather than the entire course of the program.
Guidance on assessing potential ROI of EBPs
- Triple Aim: Meeting the Triple Aim of Health Care Reform describes methods to evaluate quality, costs of the CDSMP program. Triple Aim–related outcome measures include:
- better health (eg, self-reported health, pain, fatigue, depression)
- better health care (eg, patient-physician communication, medication compliance, confidence completing medical forms)
- better value [eg, reductions in emergency room (ER) visits and hospitalizations in the past 6 mo]
- Practical Cost-Benefit Analysis: This paper describes how to conduct a practical cost-benefit analysis using falls prevention EBPs as an example.
- Cost-Minimization Analyses: While this paper describes how to do an economic analysis from a health system perspective, it still provides useful methods for how to incorporate implementation costs, outpatient costs, and inpatient costs if you have access to this health care data.
Getting Started with the Program to Encourage Active, Rewarding Lives for Your Community
These are questions related to what’s required to create PEARLS™ and how to get started in providing a program in your community (e.g. staffing, funding, and resources)
I'd like to consult with your team about providing PEARLS™ in my community. Can we meet?
Our team hosts weekly “office hours” and can answer any questions related to development and implementation of PEARLS™. Schedule a meeting time. You may also send any individual specific questions via email to uwpearls@uw.edu.
Can we provide PEARLS™ in a group setting?
Some organizations offer PEARLS™ in a group setting and are finding great success. There are some considerations when offering the program in this setting. View our list of considerations here. For access to additional resources received from and designed with other organizations (group agreements, agendas, flyers, etc.), contact us with PEARLS in Groups in the Subject line.
Please note that PEARLS™ is only evidence-based in one-on-one settings.
Can we provide PEARLS™ by phone or virtual formats?
Yes, you may deliver PEARLS™ by phone or virtual formats. Several organizations offer via phone or online as the program sometimes is more accessible via these methods. Depending on your client, it may be helpful to have the first session or baseline session in person or drop materials off in person if your coach feels it would be helpful in building rapport. Confidentiality re) any sensitive information should be maintained, so consider online platforms and secure phone lines when coaching in by phone of in virtual formats.
When offering by phone or online and if your participant is hard of hearing, consider providing some tools to ensure good communication, e.g. putting the phone up to their ear, rather than on speaker, and/or using headphones. Some hearing aids may even connect to a phone. With phones, we’ve learned both that the phone can make people more comfortable to share, or the opposite.
For paperwork like the PHQ-9, it may also be helpful to mail or email your participant cue cards or an empty copy of the questions/answers and the PEARLS™ worksheet. If they feel comfortable, they can write along with you so that they have a copy of their goal/plan/activities after each session.
Can we provide PEARLS™ in languages other than English, and do you have resources in languages other than English?
Yes. There are organizations that offer PEARLS™ in languages other than English.
In practice, PEARLS™ has been successfully implemented with Chinese, Vietnamese, Korean, Filipino, Russian, and Latino elders using either bilingual and bicultural PEARLS™ coaches or trained interpreters.
We have translated some of our PEARLS™ materials into other languages, including Chinese (Mandarin), Farsi, Korean, Russian, Somali, Spanish, and Vietnamese. We also recommend reviewing translated materials with native speakers from the community to ensure that the language is appropriate. Access our translated PEARLS™ form here.
The PHQ-9- the questionnaire used to measure individual progress during PEARLS™ sessions) is offered in more than 80 languages.
Contact us to request copies and/or links to materials.
Can we provide PEARLS™ for those who are in recovery for sobriety?
PEARLS™ does not require a participant is sober but rather that they are not functionally impaired by their substance use. If the participant is motivated and sober, it would be appropriate for them to engage with PEARLS™.
Ultimately it is up to you and your organization whether you engage this client in PEARLS™. We don’t have hard and fast rules re) prospective participants in recovery or their length of time in recovery and the option to engage in PEARLS™.
PEARLS™ is not a replacement for SUD treatment and their sobriety journey, but PEARLS™ tools can help support the participant in creating a new normal now that they are sober (e.g., PST to problem solve new social activities that don’t involve drinking, ways to stay connected with people in their life, etc.). Additionally, the PEARLS™ program can determine that the participant needs to be actively engaged in some substance use program in addition to PEARLS™ to support their recovery and to provide a resource for crises that may arise and be outside the scope of PEARLS™. This would be similar to how at times, organizations require PEARLS™ participants with severe behavioral health problems that might need 24/7 crisis support to be enrolled in additional BH treatment outside of PEARLS™.
We recommend having a plan in place (safety planning upfront, including w/participant), especially if the participant resumes drinking and comes to sessions intoxicated.
Can we provide PEARLS™ for people with intellectual disabilities?
There hasn’t been any research done regarding PEARLS™ and older adults living with intellectual disabilities. However, the overall thought is services should be approached with the same considerations when using PEARLS™ with someone living with a substance use issue, schizophrenia, etc.
That is, consider the level of intellectual disability of the individual, and if they would be able to fully participate in the process. Because the PEARLS™ program requires critical thinking it may not be a good fit for some, but others may find it very helpful.
Can we provide PEARLS™ for people with mental illnesses?
PEARLS™ could welcome those with serious mental illness (SMI). These could be individuals living in community housing, including some individuals receiving psychiatric services and a small proportion attending psychosocial treatment programs. Many may be socially isolated, and many or most do not receive services in the homes.
The initial eligibility criteria were partially based on the original research study design (to isolate PEARLS™ impact on people living with depression and not co-occurring MH/SA conditions), and partially based on training up social workers/CBOs who may not have regular clinical support to support people living with SMI.
Serving individuals on a case by case basis would be ok, if the organization is well suited to integrate PEARLS™ into their toolbox as a way to reach older adults that don’t have access to other care, plus offer additional clinical support if needed for other mental health issues besides depression (or with depression, such as supplementing PEARLS™ with anti-depressant Tx). A best practice plan would be to involve training staff and peers serving these individuals in boarding homes, supported housing, and other community housing setting where they live semi-independently.
Someone living with bipolar disorder is a little more nuanced. They can still be involved with PEARLS™ as long as they can fully participate and can complete the required follow up work. Those enrolled might need a little more monitoring and their Coaches may need additional support, but that is probably on an individual-by-individual basis. This is something the Coach would discuss with the individual and with the clinical supervisor. In these cases, the clinical supervision is extremely helpful in case the Coach has any questions or needs advice going forward. Some organizations have waited to enroll those living with bipolar disorder until their PEARLS™ Coaches are more experienced, but that’s not a hard and fast rule.
When can we start PEARLS™?
We recommend having coaches trained, clinical supervisors in place, funders’ approval, and the organizations’ program supervisor approval prior to the actual start of the program.
Who can be a PEARLS™ Coach?
Current PEARLS™ Coaches do not have any education or professional background requirement. Most important from our perspective are people who can build a strong, trusting relationship with a client.
In the original research studies, PEARLS™ counselors were Master’s level social workers and nurses. In today’s practice, PEARLS™ uses the term coaches and has been successfully delivered by coaches who are case managers, marriage and family therapists and other counselors, psychologists, social workers, and nurses with bachelor’s or master’s level training.
There are some organizations who are successfully delivering the program with CHWs or students. We highly recommend having someone on the team with expertise in management of depression/other chronic conditions in case someone is not improving their depression / PHQ-9 after several PEARLS™ sessions.
Coaches need to have a clinical supervisor who can make recommendations about changes to and new antidepressants, connect with client’s PCP directly about these recommendations, and assess whether other Rx are contributing to depressive symptoms, etc. This clinical supervisor could be a licensed clinical social worker (LCSW, MSW, LMFT, or LPCC), PsyD, a psychiatrist, a psych NP, a geriatrician, or a primary care physician (PCP).
For Coaches, may we utilize and train or organization's volunteers who currently work with our older adults?
Yes. Volunteers can be coaches, would complete our coach training, and can provide the program to their assigned older adults.
The challenge we hear from other organizations utilizing volunteers is that it can be challenging to ensure volunteer coaches remain and consistently serve participants for the long term. Some orgs have done this successfully.
You want to consider creating some sort of agreement with volunteer PEARLS coaches to emphasize they stay with the program for at least 6 months to a 1 year in order to minimize turnover as much as possible. Consistency and an established positive rapport with the same coach throughout the time of the program can be key to participate success.
You also want to consider thoughtfully how you can implement clinical supervision (required for PEARLS) if this will also be a volunteer.
For Coaches, what are the roles and responsibilities?
The PEARLS™ Coach’s primary responsibility is to deliver PEARLS™ program core services to the identified participant populations and maintain fidelity to the program model. Key activities for the PEARLS™ Coach include participant recruitment, assessment, and delivery of community-based direct services and interventions.
Coaches meet with PEARLS™ participants for regularly scheduled coaching sessions, either in person, remotely or in a hybrid format. Sessions may be weekly, monthly and may include follow-up calls or visits. Coaches might travel to participants home, meet participants at a mutual agreed upon location or at the community agency’s location.
Other key functions include timely completion of all documentation, compliance with data collection and submission requirements, and active participation in weekly clinical and programmatic supervision. Organizations also generally expect coaches to effectively coordinate and communicate with both internal and external providers and other PEARLS™ team members.
For Coaches, what is a typical caseload?
The average PEARLS™ caseload depends on how much full time equivalent (FTE) you have for PEARLS™ coaches and whether your coaches have other duties and responsibilities, such as providing case management services or other therapies.
Ballpark Caseload Estimate
- 15-20 participants for half-time PEARLS™ coach
- 30-40 participants for full-time PEARLS™ coach
Some PEARLS™ participants are seen for weekly sessions, while others have monthly sessions and/or follow-up calls, which allows coaches to have a bigger caseload. Other factors to consider include travel time (distance and traffic) needed to get to and from appointments with PEARLS™ participants.
Caseload sizes also vary between organizations. Some organizations span a large geographic area, which increases the travel time to see PEARLS™ participants. Not all the PEARLS™ coaches who have dispersed participants are able carry full caseloads. Some organizations have full time coaches who carry 25-to-50-person caseloads. However, another organization may have a few part-time coaches who work a total of 30 hours per week with an average of 10-12 active cases.
A tip for maintaining your caseload is to build ample time for outreach, recruitment, screening, data entry, and supervision.
Funding sources may dictate caseload size as well. Some grants or levy-funded programs aim to enroll a certain number of participants per month, quarter, or year.
For Coaches, what is a typical time commitment and coaching schedule?
PEARLS™ coaches generally meet one-on-one with older adults for eight one-hour sessions, typically over the course of four to five months. The program begins with weekly sessions that gradually taper to monthly.
Some PEARLS™ participants are seen for weekly sessions, while others have monthly sessions and/or follow-up calls, which allows coaches to have a bigger caseload.
Other factors to consider include travel time (distance and traffic) needed to get to and from appointments with PEARLS™ participants and in ample time for outreach, recruitment, screening, data entry, and supervision.
For Coaches or Trainers, does PEARLS™ require special licensing?
The PEARLS™ program does not include any special licensing for our coaches or trainers. We do not charge an annual licensing fee; our only fee is the one-time training fee for online training. Visit here for more Information about our training.
For Coaches or Trainers, does PEARLS™ require annual recertification?
We require no annual recertification. Previously trained coaches and trainers are welcome to contact us and request access to current training modules and materials, in order to refresh their knowledge and skills.
For Coach training, how do I register as an individual and pay or how does my organization register and pay?
Prospective trainees can register/pay online for training via our registration system. Payment is online via a credit card with an individual transaction for each trainee.
If you are an organization with several trainees to register and cannot pay per individual trainee with a credit card, please contact us with a request for an alternative payment method. Our team will work with you on multiple registrations and payment.
For Coach training, after registration is paid, how do I/we access and complete training?
Once trainees (or their organization representative) complete registration and payment, they receive an email giving them log in information to access the self-paced online modules. Trainees start and complete online training at their own pace.
After training is satisfactorily completed, trainees receive a link to schedule practice sessions via our online Calendly tool (dates/times are populated here, and trainees have several options for sessions). Once trainees complete satisfactorily these practice sessions, they receive notice of completion, can access the online certification of completion, and are ready to coach.
For Coach training, how do I sign up and access Practice Sessions?
Once coach trainees register and have access to PH Learn Link (PHLL), our training platform, we notify them to schedule practice sessions via our online Calendly tool (dates/times are populated here, and trainees have several options for sessions). Trainees can also schedule sessions via a link within PHLL.
For Coach training, how do I retrieve my Certificate of Completion after completing the training?
The certificate of completion is available once a participant has completed all modules, including the training evaluation. The link to download the certificate of completion is within PH Learn Link (PHLL), our training platform, directly below the large image (see below).

If participants can’t see the link, they should scroll to see if the box is checked for each section of each module (see below), as an unchecked box will not allow for a downloadable certificate. Contact us if any issues.

A clinical supervisor is required for PEARLS™. Who can be one and what makes a good one?
Clinical supervision is required for PEARLS™ and is beneficial during challenging cases, periods when a participant’s progress might slow down or recede, and behavioral issues.
Clinical supervisors should have:
- Experience working with depression and other common medications or medical conditions for older adults
- Knowledge of the PEARLS™ model (participant driven, Problem-Solving Treatment, and Behavioral Activation)
- Capability of understanding cultural issues, responses and adaptions
- Ability to not stray away from PEARLS™ techniques
- Familiarity with medications and older adult health
Supervisors can be any of the following: a licensed clinical social worker (LCSW, MSW, LMFT, or LPCC), PsyD, a psychiatrist, a psych NP, a geriatrician, or a primary care physician (PCP). In addition, for programs utilizing clinical supervisors who are not medical doctors (psychiatrists or primary care physicians), we recommend utilizing a PCP alongside of a clinical supervisor to help with reviewing medications on a monthly or emergency basis (whichever is more frequent) and/or someone with medical and medication expertise to contact in case someone is not improving after several PEARLS™ sessions or if there are concerns about high-risk medications and management of other chronic conditions.
Programs that wish to utilize psychiatrist services may find recruitment challenges due to limited funding and/or availability. Ideas for connecting with psychiatrists include contacting an academic medical center or university that has training as part of their mission.
For clinical supervisors, what training and resources do you provide?
We have recorded online clinical supervisor training led by a geriatric psychiatrist & local clinical supervisor and slides. For access to these materials, contact us.
We meet w/clinical supervisors once a month online to provide support and answer questions and create community among these professionals. The supervisor will receive an email invitation to attend. Participation is encouraged and optional. Supervisors may also share resources directly with the clinical supervisor group or to our larger partner group that meets monthly.
Some sites prefer to also have their clinical supervisors take the PEARLS™ coach training – not necessarily going through the full training (though they are welcome to), but to have access to the more detailed modules. If you’d like that, the clinical supervise should sign up and register like a PEARLS™ coach would here.
For clinical supervisors, how do we utilize them and how often are they needed?
When a program first begins, clinical supervisors can review training materials and practice PEARLS™ techniques with the PEARLS™ coach. After PEARLS™ sessions pick up, PEARLS™ coaches can work with the clinical supervisor to discuss whether a person referred to PEARLS™ is appropriate for the program, discuss how to support participants who are not improving their depression, recommend medication management if needed, and other services or support.
Clinical Supervisors engage in the following:
- 90-minute sessions 1x/month for small caseloads
- 90-minute sessions 2x/month when caseloads pick up
The frequency of supervision depends on the number of coaches and participants they have so if monthly isn’t enough to review new participants and participants who are not improving their PHQ-9 after several sessions, they can meet more frequently with their clinical supervisor who is not a doctor and then meet every other month with the doctor.
For clinical supervision, is it okay to have more than one supervisor who share a caseload?
Yes, it’s okay for programs to have multiple clinical supervisors especially if it allows them to get medical expertise to advise coaches on things like medications the PEARLS™ participant is taking (for depression or for other health conditions, that may bring side effects that are similar to or exacerbate depressive symptoms).
Some programs use clinical social workers or psychologists for PEARLS™ supervision and meet less frequently with a primary care provider to review medications. Another strategy one organization uses when a doctor is not available for regular supervision is to share the medication lists for new participants for the doctor to review “offline” (e.g. not during a live supervision session) and to reserve live clinical supervision time for consultation with coaches.
For clinical supervision, can we provide it remotely?
You can provide clinical supervision over the phone or by video conference. The clinical supervisor does not have to be local. If possible, we recommend group supervision where one clinical supervisor meets with multiple PEARLS™ coaches (from your organization or with coaches from other organizations). This can provide peer learning and support, along with knowledge from the clinical supervisor. It can also potentially save time and money.
For clinical supervision, do we need to carry medical malpractice insurance?
Organizations should have some form of insurance since they are providing depression treatment (which unfortunately brings small risk of being sued ); however, it does not have to be medical malpractice insurance unless the clinical supervisor is a clinician and they are delivering PEARLS™ out of a clinical setting. Other insurance is typically called liability insurance.
The insurance coverage can be whatever liability coverage your organization provides, which in some cases is liability insurance and in other cases includes medical malpractice insurance. What typically goes into this decision is: 1) the way the PEARLS™ program is classified (clinical, non-clinical, educational) which is often vis a vis how they are funded, and 2) what the insurance carrier says.
For clinical supervision, what can we expect with cost and funding for a clinical supervisor?
Rates for a clinical supervisor may vary locally from $150-$200 dollars an hour. Look into funding opportunities with organizations and county agencies that work with older adults.
A contract is helpful in order to establish supervision goals, hours, and rates. It also makes clear that PEARLS™ clinical cases are not part of the supervisor’s clinical responsibility.
For more details about PEARLS™ funding options, see the related FAQ.
What are the roles and responsibilities of a Trainer?
PEARLS™ trainers can train others in-person with or without the modules in our online learning management system PH Learn Link. We provide materials/handouts and other guidance for trainers to facilitate a 2-day training in their community.
We’d like trainers to apply their training skills soon after they learn them and get support in training for the first time. So, we ask new PEARLS™ Trainers to deliver a PEARLS™ training with a co-trainer within 6 months of being trained.
Trainers periodically report to UW how many people they train + share trainees’ emails so we can add them to our listserve and invite them to monthly TA calls, etc. We also invite new PEARLS™ trainers to facilitate our practice sessions for coaches trained online through our Coach training. New trainers are not required to do this but it’s a great way to build and keep up skills, and we appreciate having new trainers who bring different skills and experiences to the PEARLS™ family. For the practice sessions, trainers are paid for their time, and the commitment is up to them (1-4 90-minute Zoom practice sessions per year).
How can I become a Trainer so that I can train others to be PEARLS™ Coaches?
Participants in Train the Trainer (TTT) must have been a PEARLS™ coach, have enrolled 10 PEARLS™ participants as a Coach, and taken our Coach training at $500 per person. There are some exceptions (e.g., if a program manager has been managing PEARLS™ coaches for a long time and has been a trainer for other EBPs). We also generally recommend organizations have been offering PEARLS™ for at least a year before enrolling in TTT, so that it gives them time to really establish the program, problem solve and have enough experience and organizational systems set up.
The series is offered every 12-18 months depending on demand. We schedule these based on interest. Train the Trainer is an additional $700 per person for this training. ($750 if we need to provide hard copy materials). Rates quoted are 2025-2026 and may increase. To be part of the future training and receive updates on when these are scheduled:
What is the time commitment for staffing PEARLS™ (coaches and program and clinical supervision)?
The following are time estimates for staffing a PEARLS™ program. Estimate does not include the six to eight PEARLS™ sessions offered for individual participants or in a group setting.
- Clinical Supervision: 1 – 4 hours per month per PEARLS™ coach/not per participant (each participant is usually only covered a few times during supervision)
- Program Supervision: 1 – 4 hours per month per PEARLS™ coach (many programs meet with a program manager and other coaches or counselors on a regular basis)
- Travel Time: Calculated per PEARLS™ participant. Travel time is difficult to estimate because the distance and/or traffic between the PEARLS™ coach and participant varies greatly, along with how frequently they are meeting (e.g., they may meet for four hours in the first month for weekly visits, but switch to meeting one hour per month)
- Paperwork: 15-30 minutes per PEARLS™ participant per session (this also depends on the organization’s requirement for entering information into a data management system)
- Recruitment: This is more per PEARLS™ coach (or program staff in some cases) than per participant. Recruitment can be 1-4 hours per week on presentations, meetings with clinics and/or community-based organizations, etc. Time can also depend on whether you already have relationships with referral organizations or partners.
- Screening: 1 hour per potential participant (a depression diagnosis is not needed)
What is the cost of providing PEARLS™ and funding options?
The main costs that organizations pay to do PEARLS™ is staff time – delivery of PEARLS™ sessions and outreach, screening, and any administrative tasks. Costs can vary from organization to organization, depending on how much your staff time costs to deliver the program (factoring in time for recruitment, transportation, and time with the clinical supervisor), whether they are working part-time or full-time to deliver PEARLS™, and how much the clinical supervisor’s time costs.
Organizations often pay an external clinical supervisor for several hours per month for task shifting and sharing. The other cost is that there is a one-time payment for PEARLS™ coach training ($500 per person), and we can work with organizations on economical payment plan). We also have a train-the-trainer model to build local capacity to sustain PEARLS™. For more info on our Train the Trainer program, visit here.
A general estimate is $1,350 or a $150 per unit rate for nine sessions (eight in-person sessions, along with one screening and follow-up). This is based on the unit rate that the state Medicaid waiver uses in Washington, as well as what we’ve learned from several other programs.
Potential Funding Sources
Listed below are the different funding sources that organizations typically use to support PEARLS™ delivery However, not all of these are available in all states, some funding options cover multiple programs, so organizations have to decide whether to fund prevention or depression, and many options are short-term (1-3 years) vs. sustainable funding. Please note that some of these sources may no longer be active.
- Older Americans Act (OAA) Title III Part D Disease Prevention and Health Promotion (III-D)
- These federal funds are distributed to State Units on Aging who then distribute them to AAAs within their state, the amt is based on population formulas
- The funds are used to support evidence-based programs (EBPs) like PEARLS™, and can be used for multiple EBPs
- E.g. VINE Faith in Action is a community-based organization (CBO) in rural Mankato, Minnesota that gets Title III-D funds through their partnership with their local AAA
- Grants and Foundations
- E.g. 2024 Administration Community Living (ACL) Chronic Disease Self-Management Education (CDSME) grant to Trager Institute in Louisville, KY
- E.g. 2023 ACL CDSME grant to New Mexico Diabetes Advisory Council/NM Dept of Health
- State and local funding
- E.g. Veterans, Seniors & Human Services Levy – AAA and CBO (African-American Elders Program and IDIC Filipino Senior & Family Services) partnership (WA) 2024-2029 implementation plan
- E.g. Mental Health Services Act (MHSA) Prevention & Early Intervention (PEI) – funded by a 1% tax on people with incomes over $1 million (hence the nickname, the Millionaires Tax), MHSA funds 25% of public mental health services in California. County mental health agencies contract with CBOs to reach older adults historically underserved by the mental health care, choosing which programs to deliver based on stakeholder engagement and gaps in care. For example in San Diego, the Union for Pan Asian Communities (UPAC) receives MHSA PEI funds from the county mental health department to deliver PEARLS™
- Medicaid, Medicaid Waiver, Medicare Advantage Plans
- E.g. Maryland’s Total Cost of Care Model – health care systems pay for MAC AAA and other CBOs to provide PEARLS™ to their patients to improve access to quality mental health care in Maryland
- E.g. 1115 Medicaid Waiver for home and community-based services (HCBS) clients who qualify for COPES personal care services to support aging in place – the Seattle-King County WA AAA contracts with a local CBO Sound Generations to delivery PEARLS™ using this funding
- Non-profit Hospital Community Benefits
- E.g. Texas Health Resources (health system) partnership with AAA, faith community nurses, and community health workers to deliver PEARLS™ to under-resourced zip codes in multi-county region in North Texas
- Often, PEARLS™ uses multiple sources of funding
- The Harvard Community Senior Center in McHenry County, Illinois uses funding from the center, Advocate ~ Aurora Health System, the McHenry County Mental Health Board, and a Senior Services Grant
What information is helpful to provide when we are completing funding and grant applications?
When providing information to organizations for funding and grant applications, include as much PEARLS™ evidence as possible. You can find this information on our website. If you need additional resources, please contact us.
Providing PEARLS™ in Your Community
These are questions about PEARLS™ coordination and operations.
Can we do a rolling enrollment or do we need to have one cohort?
We encourage you to stagger your PEARLS™ participants – this will help with your workload since PEARLS™ sessions start off weekly and taper off to monthly. Thus, you can still be recruiting some folks as you’ve enrolled others. Staggering PEARLS™ participants will allow you to guide more PEARLS™ participants at the same time with a more consistent workload across the few months and also helps since it’s likely you will have folks referred to you at different times of year.
How can my organization screen older adults for depression?
Some organizations currently screen for depression as part of their annual assessment or intake. If you do not already do this, you can add a brief, validated depression screening instrument (such as the PHQ-9) to your practices, which will be key to identifying older adults who may be eligible for PEARLS™.
How can my organization measure individual progress or outcomes?
The University of Washington Health Promotion Research Center (HPRC) provides questionnaires to measure progress or outcomes for individual PEARLS™ participants. We will go over the questionnaires during training and provide the needed materials in the PEARLS™ Implementation Toolkit.
- Baseline and Final PEARLS™ Questionnaire: This questionnaire includes measures for self-rated health, physical activity, social activity, and pleasant activities. They help establish where the participant is when they begin the program and where they are at the end.
- Session Questionnaires: For each of the PEARLS™ session you will use what is known as the Patient Healthcare Questionnaire (PHQ-9). It is a brief, validated measure of depression severity used in primary care. It consists of nine questions that measure how much someone’s symptoms of depression (e.g., low energy, lack of appetite, depressed mood) are affecting them. Administering the PHQ-9 at each PEARLS™ session provides a way to monitor a participant’s progress throughout the program, as well as educate them about their depression symptoms. Depression outcomes include:
- Remission (no longer meets criteria for clinically significant depressive symptoms)
- Response (≥ 50% drop between baseline and final PHQ-9 score)
- Significant Change (≥ 5-point drop between baseline and final total PHQ-9 score)
- Participant Satisfaction Questionnaire: This allows you to see how participants felt about PEARLS™, gather quotes and reactions, and evaluate where there are areas for improvement. In addition to this questionnaire, we encourage agencies to gather testimonials from participants to use for program evaluation and marketing.
These individual outcomes can be looked at collectively on a regular basis to show your organization’s impact, including the quarterly change in PHQ-9 scores for all PEARLS™ participants and/or the percent of participants that met remission each year.
How can my organization evaluate the overall program success?
In addition to individual outcomes, it is important to assess how well PEARLS™ is being implemented overall. This includes looking at the percentages of people that move through the program, such as referrals, people who enroll, people who complete the program, and people who enrolled but did not complete the program. You will also want to look at whether key program components are in place, such as regular clinical supervision meetings.
The PEARLS™ Implementation Toolkit offers one model for evaluating program implementation, including examining program reach, effectiveness, adoption, implementation, and maintenance.
Sticking to the PEARLS™ Protocol and Model
We have developed a tool to help organizations assess whether they are staying within the PEARLS™ protocol and model (referred to as program fidelity). PEARLS™ coaches or program supervisors can use this brief instrument. We published a research article about the development and testing of the fidelity instrument. A link to the instrument we tested can be found along the right-hand side of the research article webpage (Click “Open Supplemental Data”).
The PEARLS™ Implementation Toolkit includes a coach self-assessment as well as a checklist to help coaches remember key components of sessions.
Please contact us with any questions about fidelity and balancing fidelity with program adaptations.
How can my organization collect, track data and manage case records for PEARLS™?
Regular data collection is important for monitoring individual PEARLS™ success and adjusting as needed. Tracking data also allows an organization to monitor and evaluate the program’s benefits and challenges. See below for some possible data tracking options. PEARLS™ does not require one specific data management system as we understand that some organizations are required to use their own internal systems; others may choose to use other options used by PEARLS (e.g. WellWare or Excel).
- WellWare: We teamed up with Sound Generations to create this online data management system. Its features include tracking referrals and participants, process and outcome reports, and downloadable forms in Word and PDF format. The system is built on Salesforce’s secure cloud platform that is widely used in healthcare, financial industries, and government agencies.
- Cost: $200 per year per single user license (2025 rates; rates may change)
- Contact: Meghan Thompson, Sound Generation
meghant@soundgenerations.org
206-268-6701 - PEARLS™ Provided Resources: We provide a survey data excel sheet in the PEARLS™ Implementation Toolkit.
- Develop Your Own Excel Sheet or Use Your Existing Data Systems: Some organizations have developed their own excel sheet(s) to track PEARLS™ data, while others use their existing data systems, such as ReferNET or PeerPlace databases.
Are we required to use your standard PEARLS™ Forms?
We do not require you to use our PEARLS™ forms; however, they may be useful if your organization has no existing similar forms. That being said, we recommend including the following PEARLS™-specific items on any consent forms:
- Include wording about PEARLS™ services (does not necessarily need to be from our example)
- Release of patient information to primary care provider and the clinician overseeing your PEARLS™ program if your client is willing
- Possibly sharing de-identified data for your institution to analyze for quality improvement or evaluation, or for research purposes if your client does not opt out of data sharing
- Convey that anyone participating in PEARLS™ recognizes the program is about skills building (problem solving and scheduling pleasant, social, and physical activities) to help improve your mood and energy – or whatever language you feel will best convey these concepts.
If you plan to use the PEARLS™ logo on your organization specific forms, request approval for use of the logo here. You will be asked to acknowledge and accept our Logo Use Guidelines.
For the consent form, is it okay to alter some of the language?
You are welcome to change the language in the consent form, as the form is a starting point from which your organization can work. We don’t require you use the word depressed, so you are welcome to edit your consent form to remove that word. You may also edit the consent form to include hybrid PEARLS™, over the phone PEARLS™, PEARLS™ at a park or in public spaces, etc.
We recommend including the following PEARLS™-specific items on any consent forms:
- Include wording about PEARLS™ services (does not necessarily need to be from our example)
- Release of patient information to primary care provider and the clinician overseeing your PEARLS™ program if your client is willing
- Possibly sharing de-identified data for your institution to analyze for quality improvement or evaluation, or for research purposes if your client does not opt out of data sharing
- Convey that anyone participating in PEARLS™ recognizes that the program is about skills building (problem solving and scheduling pleasant, social, and physical activities) to help improve your mood and energy – or whatever language you feel will best convey these concepts.
If you plan to use the PEARLS™ logo on your organization specific forms, request approval for use of the logo. You will be asked to acknowledge and accept our Logo Use Guidelines.
For the PHQ-9, what are some tips for administering the questions during PEARLS™ sessions?
We recommend having the PEARLS™ coach read the nine questions in the PHQ-9 as stated on the form to ensure you are sticking to the PEARLS™ protocol and model (referred to as program fidelity).
The name PHQ-9 may not mean anything to PEARLS™ participants. Some PEARLS™ coaches refer to the PHQ-9 as the nine questions that they ask at the beginning of each PEARLS™ session to see how the participant is doing since they last met. As participants get more comfortable doing the PHQ-9 and talking about depression, the questions become a tool for teaching them about their symptoms of depression and how to monitor them (like with monitoring their blood pressure or sugar for people living with hypertension and diabetes).
Yes/No Framing and Using a Scale
It may be easiest to phrase PHQ-9 questions as a Yes/No and use visuals to help PEARLS™ participants answer, such as this visual scale or a calendar to display the past two weeks.
Timing
We recommend that coaches administer the PHQ-9 at the beginning of the session. However, participants may have a strong desire to talk about particular topics or events, so it is okay to catch up a bit and then administer the PHQ-9.
Additional Resources
More tips about administering the PHQ-9 can be found in the PEARLS™ Implementation Toolkit’s section on PEARLS™ sessions.
For PHQ-9 screening, may we repeat screening, especially if we suspect the prospective client would benefit from PEARLS™?
The PHQ-9 typically asks for a previous 2 week view of symptoms. If you would like to repeat the screening, we recommend waiting at least 2 weeks before repeating. That said, you can also make the case that since the client is being asked about the prior 2 weeks – not just their mood symptoms on the day of the screen – then it would not really matter as much if they were having a “good day” on the day of screening. They’d really need to have had a good week to really score too low.
What if a participant's PHQ-9 score does not improve or worsens?
Consult your clinical supervisor about how the PEARLS™ participant is doing with their Problem-Solving Treatment and Behavioral Activation. Work with the clinical supervisor to examine other things that could be affecting the participant’s depression.
Score Fluctuation
PHQ-9 scores may fluctuate both ways — e.g., some participants may start with a very high score and drop significantly after the first session, while others may increase after the first session. In some cases, the fluctuation in scores may be affected by how comfortable the participant is with answering the questions, whether they believe their score is tied their ability to continue to receive services, their increased awareness about depression, and/or how long it takes them to perceive a benefit from someone visiting their home.
It may be that the participant is working on problems and activities that are not central issues to their depression. Try to explore deeper problems that they may want to address.
At times the total PHQ-9 score stays the same but there may be improvements in some of the questions and decreases in other questions. A participant’s score could also stay the same even if they have made positive changes in their lives. Remember to point out the participant’s successes, even if they are small.
For clinical supervision, why do we do medication reviews and collect medical info on the Participant Information form?
While PEARLS™ is not a medication management program, medical reviews have sometimes identified medications a participant no longer needs or some medication interactions that could be considered by a pharmacist or primary care provider. Additionally, it can be helpful to have a clinical supervisor review medications in case a participant is not getting better with PEARLS™. In some of the early effectiveness trials and based on what other orgs have done, we have seen that some participants adjust their antidepressants or go onto antidepressants over the course of the program. For this reason, it can be helpful to have someone reviewing medications. For example, some orgs will pair their LCSW and have a PCP review meds annually.
All of that being said, we support what works best and is feasible for your organization. If it’s not feasible to have someone reviewing medications regularly or annually, then it may not make sense for you to collect this information. Instead, you might adjust, such as gathering whether or not someone is taking psychiatric medicine and how frequently.
From a research perspective, we do not require this information. This information is meant to be functional in order for you to offer PEARLS™ and gather the information you need to support your participants.
For serving participants who are suicidal, are there resources and/or strategies?
Within our online Coach training, we do address suicide and self-harm. Beyond the training module, we do not have any specific assistance around suicide.
Some online resource materials might be helpful to you.
- Our first PEARLS™ Connect paper
- This article from the American Society on Aging
- We have 3 additional resources around suicide protocols and if someone endorses a 1,2,3 on Q9 on the PHQ-9 that might be helpful. Please contact us to request these resources.
For serving participants who are visually impaired or blind, are there resourcs?
The Sacramento Society for the Blind serves blind participants. Their staff suggests, in general, that if materials are in Word and if the person knows how to use a screen reader, then many documents will be accessible. Programs can also translate materials into Braille and/or use voice recording. Recording may be helpful in explaining the 7-step problem solving method or recording goals and steps.
Illinois organizations can check in with The Chicago Lighthouse.
For serving participants with dementia are there resources?
We have materials that provide some guidance and best practices. Please contact us to request these resources. If emailing please include Dementia Resources in the subject line.
Can we repeat or pause PEARLS™ sessions?
Setbacks can create scheduling issues or disrupt the frequency of sessions. When a trauma happens in the middle of PEARLS™ sessions, work with your clinical supervisor to possibly meet the participant more frequently to get on top of the new problem or setback.
It is okay to pause PEARLS™ sessions for one to two months if a participant is away or in the hospital. When resuming sessions, you may need to meet more frequently at first to get the participant back on track. You are still aiming for a total of eight sessions.
After a setback, resume weekly sessions initially to reinforce skills even if the participant is further along in the program.
If a caseload permits, it is okay to repeat PEARLS™ a second time. If the participant is requesting to go through the program a third time, there may be other underlying issues that need to be addressed outside of PEARLS™, including that some participants enjoy having a visitor. Many communities offer free services for friendly visits.
For disenrolling participants, what is the protocol, i.e. deactivating them from our program and reflecting this in our records?
We understand that participants may enroll, participate in one session or less, and then not be in contact with your, regardless of your efforts to reach them. Our inclination is to use “declines to participate” as this is ultimately the reason they are no longer active.
However, there’s no pre-determined language when recording participant disengagement and then subsequent disenrollment from your program. The reasons can vary by organization. So, it depends on how your organization wants these tracked.
For participants who are ineligible to participate in PEARLS™, what and how should we communicate this to them?
This kind of communication is usually done as a discussion, either over-the-phone/Zoom or in-person immediately after the screening tools have been completed. However, if you need to create a follow-up letter, definitely phrase it as something like: “based on what you’ve told me for these different screening questions, PEARLS™ is probably not a good fit for you at this time.” It’s always that PEARLS™ isn’t a good fit for them, NOT that the person is not a good fit/eligible for PEARL, i.e. never the person’s fault. You can also share other resources and refer participants to other programs or services (internally or externally) that might be a better fit for that participant.
For participants who are not responding to a 3-4 month follow-up after their final session, what can we do?
Try sending a reminder letter with the coach’s contact info and date/time of the follow-up call or have a backup person with contact information who can help get in touch with the client-if the PEARLS™ participant is comfortable with this.
When you do get in touch for the monthly check-up, schedule out the future calls while you’re talking to them – this at least gets it on the calendar, and then future outreach can be reminders about the already scheduled call.
Lastly, from a data perspective, it is okay if you tried to get in touch but have been unable for various reasons. You may not be able to gather 6-month follow-ups for everyone.
What is the eligibility criteria for serving a person who is primarily dealing with social isolation?
For the PEARLS™ Connect Study, we only included older adults with depression as we were partnering with PEARLS™ programs who are funded to serve this population. In practice, PEARLS™ programs screen for depression differently – some use a cut off of >/= 10 on the PHQ-9, others use the criteria you mentioned below (at least a 2 or 3 on Q1 or Q2 cardinal symptoms, with at least 2 total symptoms a 2 or a 3.
We did not screen for isolation or loneliness – instead, all PEARLS™ participants were invited to participate in the study and complete several brief social connectedness surveys – the Duke Social Support Index-10, the PROMIS-6 social isolation, and the UCLA-3-Loneliness.
We then tracked changes in social connectedness 6-months following enrollment (after PEARLS™ in-person sessions ended) and 12-months following enrollment (6-months following completion of the working sessions).
At enrollment, PEARLS™ participants were on average less connected then the general older adult population but we didn’t screen people in or out based on the social connectedness surveys.
We don’t really know how PEARLS™ would work to reduce isolation or loneliness among people who are not depressed. However, in summer 2025, our team began to explore further social isolation and PEARLS™ and applied for grant funding.
Do PEARLS™ coaches have to do both Problem-Solving Treatment and Behavioral Activation during each session?
While we encourage and teach Problem-Solving Treatment and Behavioral Activation (social, physical, and pleasant events scheduling) at each PEARLS™ session, it is okay if only one happens during a PEARLS™ session given other circumstances.
Some participants are resistant to doing Problem-Solving Treatment because this type of approach is not something they are familiar with or does not resonate with their worldview. One way to address this is to teach problem-solving skills using barriers that come up when doing Behavioral Activation. For example, if the participant is unable to walk around their neighborhood because of safety concerns, the PEARLS™ coach and participant can work through seven problem-solving steps to identify other ways to be physically active such as walking during the day with a neighbor or doing seated exercises in their living room.
Other participants might prefer to just work on only Problem-Solving Treatment, skipping a physical activity for that week, for reasons such as feeling ill.
Do you have to do all of the legs of the PEARLS™ stool during each session?
No. While we encourage and teach PST and behavioral activation (social, physical and pleasant events scheduling) at each PEARLS™ session, it is OK if only PST or BA is worked on during each session given other circumstances. Some participants are resistant to doing PST because this type of approach to problem-solving is not something that they are familiar with or does not resonate with their worldviews. Some participants are feeling ill may prefer to just work on PST and not plan a physical activity for that week.
Remember, the clinical supervision (the floor of the PEARLS™ stool) is required as it provides regular support for the PEARLS™ coaches, timely responses to questions about eligibility, what to do if a participant is ill or needs to pause the program, and how to work with participants who are not improving their PHQ-9 scores after several sessions.
For participant sessions with coaches, may we record them for the purpose and quality control and Coach review?
Our consensus is that recording a session is fine as long as the participant and any funders are aware and consent to the arrangement. We recommend putting this agreement in writing between the coach and participant during the initial intake session.
Can participants who have completed the program continue with or repeat PEARLS™?
Continuing or repeating the actual PEARLS™ program is not really a goal of the program. However, if participants still need more help with their depressive symptoms/ learning the process, then we believe it would be fine for them to continue doing PEARLS™ – this is your agency’s decision to make.
If participants want to stay involved in general, then your agency could:
- Refer participants to other, similar programs in your area. Participants could research these as an active task to complete.
- Start a post-PEARLS™ support group to help address this need for ongoing support. These support groups are a way for PEARLS™ graduates to connect, maintain skills, problem solve together, etc. Some are led by PEARLS™ coaches; others are integrated into their existing support/activity groups. These are not officially PEARLS™ per say but can be a way to provide ongoing support w/ depressive symptoms and learning the process. Some do periodic PHQ-9s to evaluate whether participants are maintaining their improved depression. We don’t manage the post PEARLS™ support groups; however, we recognize these as very cool adaptations that organizations have come up with organically.
Some organizations have successfully implemented post-PEARLS™ support groups. If you would like to connect with these organizations contact us for these referrals.
When serving participants, what home safety issues should staff and participants be aware of?
Some safety issues staff can assess and should be aware of:
- Are there animals in the home, bug infestations, or weapons (if yes, ask about gun safety measures). A “Yes” doesn’t keep staff from meeting in the home but might affect whether they wear more protective gear and will give them insight to access.
- If participants feel safe in their home: community and fall risk/trip hazards.
- If participant has increased thoughts of suicide/self-harm.
- Some isolated adults may have bedbug or insect issues. Coaches should bring minimal things such as their own chair and spray down their stuff with alcohol. You could also try to meet elsewhere that is close by and private.
For medical safety (e.g. COVID, flu, etc.), coaches can talk to participants about the decision whether to wear or not to wear masks. As coaches work with many older adults, they don’t want to accidentally pass on illness (Covid, flu, etc.), though we are aware that because some people are hard of hearing it might be preferred for them to be able to see mouths vs. listen to someone masked. Staff can let participants know they are fully vaccinated against certain illnesses (e.g., COVID), even if not required to do this in their organization’s workplace. This allows participants to weigh risks of participating in person.
Can my organization provide other therapies during PEARLS™ sessions?
The original PEARLS™ research focused on two evidence-based treatments — Problem-Solving Treatment (PST) and Behavioral Activation (BA). We encourage PEARLS™ coaches to stay focused on delivering those two treatments during PEARLS™ sessions to teach older adults skills to manage their depression.
Why just those two?
If you do other treatments during PEARLS™ sessions, you can never be sure that you are giving someone an adequate dose of any psychotherapy, and the evidence-base requires a certain amount of Problem-Solving Treatment and Behavioral Activation.
When are other psychotherapies okay?
It is okay to do other psychotherapies:
- After the PEARLS™ sessions have ended; OR
- While PEARLS™ is in progress if the other psychotherapies are with a separate staff member or PEARLS™ coach AND not during the same time as the PEARLS™ session.
Can we bill Medicare and/or Medicaid for psychotherapy?
Yes, it may be possible to bill Medicare for psychotherapy. Typically, the billing codes are for collaborative care, chronic care, or psychotherapy under Medicare Advantage/MACRA or Medicaid, with clinical entities (e.g. hospitals, primary care providers) contracting with CBOs (single or network) to provide depression care outside the clinical setting. Billing Medicare and Medicaid can be a bit tricky. We are by no means experts in billing, but based on what other organizations have done in the past, we have found you need both a covered provider (e.g., licensed and independent) and Medicare billable organization.
There are distinctions between a covered provider and a billable organization. As we understand it, the covered provider is someone licensed, with the clinical expertise (e.g., LCSW) to provide mental health care; whereas a billable organization has gone thru whatever pieces needed to bill Medicaid or Medicare (e.g., liability insurance, data security/management).
To bill Medicare, one needs both; for Medicaid we believe it is just the covered provider, and in some cases, what provider is covered changes, i.e., in Washington state, the Medicaid Waiver covers PEARLS™ and CDSMP via trained human service professionals which can be basically any social service provider.
If a coach exits there position, what is a good strategy with participants while we wait for a new coach?
We recommend that coaches finish up their case load prior to leaving, especially since they have likely developed a good relationship/rapport with participants after the first few sessions. It’s best for participants if they have the same Coach throughout. During this time, Coaches can inform participants they will be leaving on X date so it’s not a surprise.
If it’s not possible for the coach to finish up cases, or if there are a few participants where coaches had only one or two sessions with them, then it’s okay to bring in a new Coach. We’d recommend a warm handoff in those cases (if possible), such as having the new Coach attend a session with the exiting coach.
How is fidelity to the program maintained?
We have developed a brief self-report fidelity instrument (20 items) that coaches or supervisors can complete; follow this link for a 2015 research article for more information about the development and testing of the tool, as well as a link to the PEARLS™ Fidelity Instrument.
The PEARLS™ Toolkit/implementation manual includes a coach self-assessment as well as a checklist to help coaches remember key components of sessions. Please contact us at contact us with any questions about fidelity and balancing fidelity with program adaptations.
Spreading the Word About PEARLS
These are questions about recruiting participants, promoting the program, and sharing PEARLS™ information with their community.
Organizations should feel free to rename the program, use a different word for PEARLS™ coaches, and/or brand the program as they see fit for their community’s needs.
Are there suggestions on how to recruit PEARLS participants?
PEARLS™ participants can come from referrals within your organization or from outside your organization. Your organization will need to create an internal pipeline for current or inquiring participants, as well as potentially cultivating community relationships for outside referrals.
Many times, the PEARLS™ coach is the person doing the recruitment, although this can vary from organization to organization.
Whoever is in charge of recruitment should be prepared with materials about PEARLS™. We recommend the PEARLS™ coach send possible participants an introductory letter once they are referred to the program. We discuss more about marketing materials in the other questions in this section.
General Recruitment Tips
Things to keep in mind with your recruitment activities.
- Build in Recruitment Time. You’ll need time to create and nurture relationships around the community. Some organizations will have their PEARLS coach hold monthly meetings with local agencies to talk about the program and referrals.
- Communicate Eligibility & Consider Your Capacity. It is important to communicate eligibility criteria for PEARLS™ and have sufficient capacity for processing referrals and enrolling new participants to ensure that referrals are appropriate and you do not discourage future referrals from your contacts. Make sure referral partners know that older adults do not have to have a clinical diagnosis of depression to participate
- Multiple Types & Points of Contact With Potential Participants. When contacting a potential PEARLS participant, it may take mailing information three times, making multiple phone calls, and/or visiting a them in-person to help them engage.
Finding Referrals
Building relationships with community-based organizations and other agencies that serve older adults and isolated populations is key to successful recruitment outside your organization. Begin networking by attending local health and aging events in your community. Connect with people from the following organizations:
- Senior Centers
- Religious Institutions
- Clinics
- Assisted Living Facilities
- Senior Housing
- Meal Delivery Programs: Meals on Wheels, etc.
- Media Sources: newspapers, TV, and radio
- Housing Authorities
- Adult Protective Agencies
- Veterans Health Administration (VA)
- Rehabilitative Units
- Addiction Treatment and Support Programs
- Emergency Responders: firefighters, 911, and/or emergency medical technicians (EMTs)
- Healthcare Providers: neurologists, primary care physicians, geriatric physicians, nurses, social workers
- Transportation Assistance Programs and Services
- Hair Stylists
- PEARLS™ Participants (they can refer friends and family based on their experience)
Promotional & Relationship Building Activities
Putting on events can bring awareness to the issue of depression and isolation for older adults and PEARLS™ as a solution.
- Hold a presentation for agencies and community partners about depression, aging, isolation, and PEARLS™. Provide food (if possible).
- Hold a presentation for potential participants on wellness education, feeling better, and/or becoming more self-sufficient or social where they could enter to win a gift if they complete a two-question survey (the PHQ-2) and provide their contact information.
- Hold a training on how to screen for depression (using the PHQ-2 or PHQ-9) and make referrals to your organization for PEARLS.
- Consider topical or timely promotion times, such as May. It is both Mental Health Month and Older Adults Month.
Connecting With a Possible PEARLS™ Participant
When you do contact and connect with a potential PEARLS™ participant for the first time, it is important to be delicate in the way you discuss and describe the program. About 75% of PEARLS™ participants do not know that they are depressed or experiencing mental health issues. Approach the initial call as if they do not know. It’s more important for them to get their foot in the door instead of convincing them that they are depressed.
After you have a referral, contact the potential participant on the phone or in-person as soon as possible (24-48 hours). Calls may take 5-20 minutes. Initial one-on-one contact could include discussing:
- The program focuses on developing skills and problem-solving to address issues that may be making them feel unpleasant or sad so they can improve their health, happiness, and quality of life.
- PEARLS™ takes place in their home or a community setting that works for them.
- The program is for older adults who might be experiencing multiple health issues, have difficult family dynamics, or want to be more self-sufficient.
- It’s a collaborative effort with a coach, and they will decide which issues in their life they want to tackle. They are in the driver’s seat.
- They will work with the PEARLS™ coach on establishing goals they want to achieve and collaboratively brainstorm ways to achieve those goals.
- While there is a fair amount of paperwork during the first PEARLS™ session, the coach will help them complete it.
Some organizations encourage the referral source to be present at the first three sessions to help build rapport and trust between the coach and participant if the participant is from a community that has had negative experiences with services or health systems.
Are there resources for recruiting participants?
We have a variety of resources available via a Google drive. To access materials go to our Google folders.
Are there tips for recruiting underserved populations?
Here are a few suggestions on how you can improve your recruiting efforts with underserved communities.
- Consider renaming PEARLS™ to something that better suits your organization or the community you are trying to reach.
- Connect with community representatives to learn how to best reach potential participants. This could include representatives from religious centers, veteran organizations, cultural centers, and/or neighborhood resources, etc.
- It is okay to use forms that have been translated and reviewed by members of the community. If you translate forms, please share them with us so we can make them available to other organizations as needed.
- Be aware that some cultures may be apprehensive about paperwork and signing documents if they have had negative historical experiences (this could include immigrants and/or Native American communities).
- Consider using words that will make sense to the greatest number of people in a community. Also think about how to best reach and connect with people who have limited-English skills.
- Make sure materials are appropriate in terms of literacy, culture, images, and spiritual backgrounds.
Are there tips for creating informational materials about PEARLS™?
Yes, we have some tips and ideas for your PEARLS™ materials.
Avoid Stigmatizing Words.You may want to avoid using the terms like depression, mental health, or counseling (or other terms you know would not resonant well with your community). You can use terms and phrases like wellness, well-being, mood, emotion, feel better, quality of life, problem-solve, skills for more independence, etc. Use terms and phrases that will resonate with the communities you are trying to reach.
Success Stories. Include success stories in your PEARLS™ materials. You can use stories from our website to help get you started.
Are there samples or templates for PEARLS flyers or brochures?
Yes, we have sample and template materials for organizations to use. They can be found here on our Google Drive. Please feel free to adapt the branding to meet your organization and community needs. You can even rename PEARLS™.
Do you have a printed brief overview of PEARLS™ I can share with my organization?
We have a brief 2-page overview of PEARLS™ that is meant to be shared with community organizations and may be helpful if there’s a center you have in mind who is interested in learning more. To request this resource contact us. You are also welcome to explore our website here.
Do you have a presentation resource we can use to introduce others to PEARLS™?
You may use our Intro to PEARLS™ PowerPoint and access our example fliers in our Google drive.
For more information about PEARLS™, watch a short video here.
Where can I find PEARLS™ participant testimonials?
Visit our website to read and view videos of success stories in PEARLS™ participants’ own words.
Do you have a media release example we could adapt to use for client photographs and videos we want to use in our promotional materials and platforms?
We do have our own UW program document to share as an example. To request this resource, contact us. If emailing us, please type Forms – Media Release in the Subject Line.
Can we use the PEARLS logo in the promotion of and within our PEARLS program materials?
The Program to Encourage Active, Rewarding Lives (PEARLS) logo is owned by the University of Washington and the PEARLS program. To use the logo, organizations must request and have approved its use, as well as acknowledge and accept our Logo Use Guidelines. Should PEARLS approve the request, PEARLS staff will send trademarked logos to the contact identified on the request form.