As published in Dimensions Magazine, Spring 2018
By Genevieve Wanucha
Resilience. The word has a certain vibrancy to it—the ability to spring back from hardship. You might be thinking of a forest growing back after a fire, or a community rebuilding after a hurricane. You might remember healing from a fractured bone or recovering from a broken heart. Resilience is generally defined as the ability to adapt to change in a positive way, cope with stress, or to thrive after trauma or illness.
In the world of Alzheimer’s disease research, resilience has a specific meaning. It applies to people who live into old age without apparent symptoms of dementia but are later found, at autopsy, to have brains with high burden of Alzheimer’s disease pathology. They are people who would be expected, by all measures, to develop the cognitive changes of dementia—and never do.
In the late 1980s, researchers suggested that these individuals have high ‘cognitive reserve,’ or the ability of the brain to find alternate ways of getting a job done despite underlying damage. Today, researchers have only just begun to work with the technologies needed to understand the genetic and biological mechanisms of resilience in Alzheimer’s disease, all the way to the level of individual neurons. Ultimately, the UW ADRC hopes to identify targets for therapeutics and find ways to promote resilience in those at risk of disease.
But, the human experience of dementia calls for a wider vision of resilience, one with relevance to the wellbeing of millions and millions of people affected in some way by neurodegenerative disease: the caregiver dealing with daily stress, the person living with memory loss who feels lonely, the daughter watching her mother change, or the young man coming to terms with his own inherited genetic risk of brain disease.
There is more than one way of being affected by dementia, and there is more than one road towards a resilient brain, mind, and spirit at any stage of life.
1. Pursue and Champion Education
Research shows that the developing brain builds a foundation of resilience through genetic and environmental factors that are, at least initially, outside of our control—better socioeconomic status, good pre- and post-natal care, stimulating environments, and education. Researchers aren’t exactly sure how education builds reserve, but they think that the cognitive and social stimulation of years of education promotes more connections between neurons. With more highways and byways forged over years, the brain can find new ways to process information if one area sustains damage from Alzheimer’s disease later in life—like a driver who can find alternate routes home in the case of a traffic snarl.

UW Medicine
Recently, new brain imaging technology, called tau and amyloid positron emission tomography (PET) scans, clarified the link between education and cognitive reserve. These scans, which assess plaques and tangles of Alzheimer’s disease in the living brain, show that the brains of highly educated people can withstand the burden of Alzheimer’s pathology for longer before developing cognitive decline than people with lower amounts of education (high school, on average). In other words, high cognitive reserve raises the threshold at which Alzheimer’s disease pathology takes its toll on cognition.
While the brain benefit of education is likely related to the higher incomes and healthier lifestyles associated with educational achievement itself, there’s more to the story.
Sources
Hoenig MC, et al. Neurobiol Aging. 2017 Sep;57:1-7.
Liu, Y., Julkunen, V., Paajanen, T. et al. Neuroradiology (2012) 54: 929
2. Mid-life Interventions
Dementia is the last stage of a process that has been going on for many years. In fact, Alzheimer’s pathology can begin to appear in the brain 15 years before the onset of memory loss. During this window, no matter one’s educational history, people who reach age 65 in good cognitive health can take actions to boost cognitive reserve and prevent the onset of cognitive decline.
“There is converging evidence that what you do in mid-life in terms of physical, cognitive, and social connectedness contributes to cognitive reserve and healthy brain aging,” says Tom Grabowski, MD, director of the UW Memory and Brain Wellness Center (MBWC)/ADRC, “and we think these kinds of factors can make years of difference in when latent Alzheimer’s disease tips into symptoms.”

Credit: G. Wanucha/ Modified w/Attribution, Slinky Toy' Andy Rogers, Flickr
The best evidence for the brain benefit of an active cognitive lifestyle comes from the Advanced Cognitive Training for Independent and Vital Elderly (ACTIVE) trial. Led by Sherry Willis, PhD, UW Research Professor of Psychiatry and Behavioral Sciences, the randomized study recruited cognitively healthy older adults who engaged in 10 hour-long sessions that trained them in skills requiring either memory, reasoning, problem solving, or speed of mental processing. Each training group showed improvements on the specific task they were trained on and reported less difficulty in everyday activities, such as managing finances or planning meals, for up to 10 years after the intervention.
In general, pursuing meaningful work is key to the health of our brains and longevity. A 2014 study out of the Mayo Clinic found that people with high scores in intellectually enriching education and occupational pursuits were more resilient in terms of cognitive decline. The researchers estimated that even for people carrying the Alzheimer’s genetic risk factor APOE4, high scores in lifetime intellectual enrichment delayed the onset of cognitive impairment by about 8-9 years, compared with lower exposure to intellectually enriching activities. Interestingly, the study also showed an independent link between higher cognition and the pursuit of activities that challenge and engage the mind in mid- to late-life.
Reading Material
Enlightened Aging: Building Resilience for Long, Active Life by Eric B. Larson and Joan DeClaire (Rowman & Littlefield, 2017)
3. Mindfulness and Meditation
Mindfulness meditation involves daily sessions of focused attention on the present, on purpose and without self-judgment. The idea is to cultivate a sense of gentle openness and detached curiosity about the here and now, including life’s difficulties. Mindfulness meditation has real-life benefits to people with dementia for several reasons.
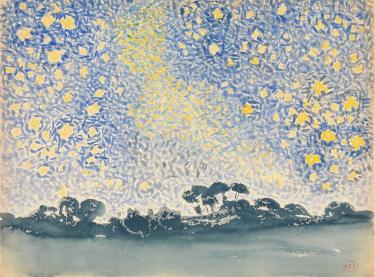
Henri-Edmond Cross. Robert Lehman Collection, MOMA
Foremost, the practice can help build mental resources for dealing with frustrations and anxiety. “Mindfulness meditation is about retraining how we respond to our environment, especially when stressed,” says Kristoffer Rhoads, PhD, a neuropsychologist at MBWC. “This becomes very important as we think about cognitive loss and anticipatory grief. It’s valuable for us to have a way to help mediate the stress response to having memory problems, to disengage from the ‘I used to be able to do this and now I can’t do that,’ to much more of an acceptance of ‘this is where I’m at right now, regardless of where I was before’.”
Mindfulness meditation is also well suited to people with dementia because the brain areas involved in tuning into the ‘here and now’ are the same brain areas that stay relatively preserved as dementia progresses. Activities that encourage mindfulness—appreciating or doing artwork, walking in a garden, listening to music, or simply watching birds in the backyard with a friend—are ones that people with memory loss can approach from a position of strength.
Caregivers, who often bear a great deal of daily responsibility, may not feel as though they can make another commitment. Yet, a robust meditation practice is worth the 10 or 20 minutes a day. After an 8-week meditation course, caregivers in a UCLA study showed decreases in markers of cellular aging (an important predictor of overall health and resilience), less distress, and better mood and thinking skills.
And for everyone, mindfulness meditation likely holds value for preventing or delaying cognitive decline, as suggested by research showing re-wiring of the brain, improved emotional resilience, and reduced modifiable midlife risk factors for Alzheimer disease, such as high blood pressure and cholesterol. What’s more, researchers saw these positive changes after 8 weeks of guided practice in people with no prior history of meditation.
“By building a habit of mindfulness at any point in life, you are putting yourself in a position to retain many important aspects of cognitive function,” says Dr. Grabowski.
Resources
The Science of Meditation by Dr. Kris Rhoads
4. Build a Powerful Caregiver Toolbox
The Memory and Brain Wellness Center (MBCW) thinks a lot about caregivers and their physical and emotional resilience.
“From the very beginning of dementia caregiving, there needs to be shift in approach from an acute illness to a chronic one,” says Marigrace Becker, Program Manager for Community Education and Impact at the MBWC. “Caregivers need a strategy for the long haul, which is an important foundation for long-term emotional resilience.”
The MBWC offers Powerful Tools for Caregivers, a free educational series at Harborview Medical Center designed to help caregivers take care of their own selves while they care for a loved one. Over 6 weeks, the group of participants builds new habits in effective communication, making challenging decisions, moving through difficult emotions and conversations, and getting connected to helpful resources.
“It’s so cool to see this switch that gets turned on for people,” says Becker. “In some cases, they may not have been thinking about themselves, and become excited about the permission to engage in self-care and seek support from others.”
From being involved in programs like this one, the MBWC team has gathered some helpful resilience-building strategies for caregivers. Be willing to be assertive and ask for help. Say no to things you can’t take on. Find creative ways to carve out pockets of time to take breaks to enjoy a hobby, eat well, and exercise.
Resources
MBWC Community Events and Programs
Sign up for Powerful Tools for Caregivers: Mondays, 4/23 - 6/4, 1:30 - 3 pm. Contact mbecker1@uw.edu 206.744.2017 See Flyer
5. Find the Right Support Group
Support groups for care partners, family members, or people living with dementia can be powerful ways to connect with others dealing with similar feelings and challenges. But sometimes, it’s difficult to find the perfect fit.
Take Laurie Bahr and the late Marty Bahr, who received a diagnosis of early-onset Alzheimer’s disease at age 50 in 1995. In Chicago, they tried several Alzheimer’s disease support groups. But they found little in common with the participants, who were all much older. The couple pushed hard at Rush University Medical Center for more recognition of younger onset dementia and services designed specifically for people who often fall ill before retirement and Medicare/Medicare eligibility, and often have children still living at home. In 2004, Rush University and the Alzheimer’s Association formed the first ever support group for people living with early-onset Alzheimer’s, Without Warning. Now, it offers a welcoming community resource to over 60 people in the Chicago area.

Association for Frontotemporal Degeneration theaftd.org
Another neurodegenerative disease called frontotemporal degeneration (FTD) can feature changes in language and emotional behavior and often onsets in middle age. For people who are caring for a parent or spouse, it can be especially important to find a support group that fits. A family going through the experience of FTD must often grieve the loss of different aspects of an intimate relationship than a family dealing with late-onset Alzheimer’s disease.
“Finding a support group that focuses on FTD is key,” says Sharon Denny, President of the Association for Frontotemporal Degeneration. “It means finding a place to mourn the loss of relationship caused by the disease, so that you can go back to that relationship with more room to be free and creative and stay in the present.” In other words, the right support group for your own family situation can foster resilience.
Resources
Alzheimer’s Association
Association for Frontotemporal Degeneration
UW Memory and Brain Wellness Center
Living with Memory Loss Handbook (UW MBWC)
6. Join Your Community

Credit: Jim Lee Carey
The concept of dementia-friendly communities is spreading around America, from Boston’s ARTZ and I’m Still Here Foundation, and Philadelphia’s memory cafés, dancing, and cognitive comedy programs, to Seattle’s Momentia grassroots movement, to name a few. Here in the Puget Sound region, people living with memory loss, their loved ones, and members of the entire community, can find a variety of dementia-friendly programs—from walks at zoos and public botanical gardens, to art classes and museum tours.
Under the banner of Momentia, these programs aim to empower people with memory loss and their loved ones to stay active and connected in the community. For people living with dementia, and their friends and caregivers, these programs can help build resilience of the brain, mind, and body through fresh air, exercise, creativity, and social time - all antidotes to loneliness, boredom and anxiety. These programs also present interested members of the public with volunteer opportunities, new perspectives, and friends.
Recently, as part of a year-long advocacy effort, members of the Gathering Place early stage memory loss program at Seattle’s Greenwood Senior Center made posters with hopeful messages of support for others diagnosed with dementia. Our team at the MBWC proudly displays these posters in our clinic. One by Jean Mills has the words, ‘It’s Hard, But We’ll Get Through It.’ “Her message touches on where resilience truly comes from,” says Marigrace Becker. “From a ‘We.’ From a connection with others.”
Resources





