By Genevieve Wanucha
“A big tangled knot” is how Linda Teri, PhD has long thought about the daily life challenges of both the person living with dementia and the care partner. This simple visual describes her approach to helping those dealing with behavioral issues, such as agitation, depression, and sleep disturbances, as well as the social factors that worsen or improve challenging home situations. Teri, now Professor Emerita in the UW School of Nursing, served in the past as Director of the former UW Geriatric Family Services Clinic, faculty in the UW Department of Psychiatric and Behavioral Sciences, and ADRC leader in medical and caregiver education for over twenty years. “I’ve always been interested in taking the knot and pulling it apart,” she says. “If you pull a few strands out, it’s still a knot, but maybe it’s less tangled. What strings can we pull from this amorphous, scary tangle of challenges that will actually help people?”
ADRC-affiliated researchers have a history of pulling on those “strings.” Starting in the early 1980s, Murray Raskind, MD, ADRC Director from 1999-2012, found that family support groups could resolve feelings of isolation and fear for spouse caregivers. Susan McCurry, PhD focused on sleep and showed that scheduled, regular exercise and light exposure during the day were powerful strategies in managing sleep disturbance in Alzheimer’s disease. Peter Vitaliano, MS, PhD studied the health effects of caregiving psychological stress and coping. Michael Vitiello, PhD studied the link between sleep disruption and cognitive changes and the use of sleep EEG for diagnosis of early Alzheimer’s disease, as well as treatments for caregiver sleep problems. Rebecca Logsdon, PhD worked with Teri and McCurry on testing behavioral therapies and teaching skills to alleviate depression and anxiety.
Through the 1980s and 1990s, the study of behaviors in the Alzheimer’s field was outside the mainstream. Teri remembers the attitude of other researchers that dementia was a cognitive disorder, so behaviors were simply epiphenomena, or by-products of a disease process: ‘Why bother studying them?’ “We were still the only group with a non-pharmacological focus on dementia behaviors,” said Teri. “At the same time, families were being told there was nothing they could do about their loved one’s behaviors, except to give medications with side effects and limited benefits.” It was this under-recognized human need that motivated her to identify the most effective strategies for caregivers to improve their home situation.
Teri began her research career at the early ADRC tracking the kinds of behavioral problems affecting research participants and their care partners who came through the Clinical Core. She soon ran into a research roadblock: there were no good measures of behavior, no scoring systems for caregiver reports about their loved one’s behaviors. This lack of objective measures limited researchers’ ability to define observable types of behaviors, rate severity level, compare groups of patients, and ultimately detect declines or meaningful improvements during an intervention or treatment study. As a psychologist, Teri also wanted a way to understand how the caregiver’s response can affect the emotional state and behavior of a person living with dementia.
Doing her homework, Teri reached out to Steve Zarit, PhD, a pioneer in the study of caregivers at Pennsylvania State University. He allowed her to use and improve his behavior measurement system: “Whatever you think will make it better,” he told her.
In 1992, Teri, along with Zarit, Logsdon, and Vitaliano, published the ‘Revised Memory Behavior Problem Checklist,’ a 24-item caregiver-reported measure of observable behavioral problems in dementia patients. Today, the tool is recommended by the American Psychological Association as a reliable and valid assessment of both the behavior problems in dementia patients, and the extent of caregiver distress related to those problems, and it has been translated into five languages.
“I think it has gotten a lot of attention because the checklist captures the behaviors and the caregiver’s reactions to them,” says Teri. Being able to “capture” a picture of the behaviors in the context of a patient’s social environment allowed her and her team to tackle those “tangled knots.” They could better identify the threads to pull to most effectively unravel the complex knot of challenges affecting care partners. These non-pharmacological approaches that grew from this foundation stand as one of the historical legacies of the ADRC and parallel efforts that have had the farthest reach into the most intimate and difficult parts of people’s lives.
Doing the ABCs
In the early years of the ADRC, Teri and Susan McCurry, now a research professor and vice chair of research at the UW School of Nursing, drew from social learning theories in psychology to create a framework for understanding the behavioral changes that occur in individuals with dementia. They called it the ABCs, where a Behavior is determined by its Activator and its Consequences. With this formula, caregivers can “get active” to change the behavior by either changing the situation that triggered it or the event that follows it. The team found that common “activators” and “consequences” of behaviors revolved around caregiver communication styles, such as arguing or holding unrealistic expectations about loved one’s ability to remember or perform tasks, which can produce a vicious cycle of worsening interpersonal conflict.
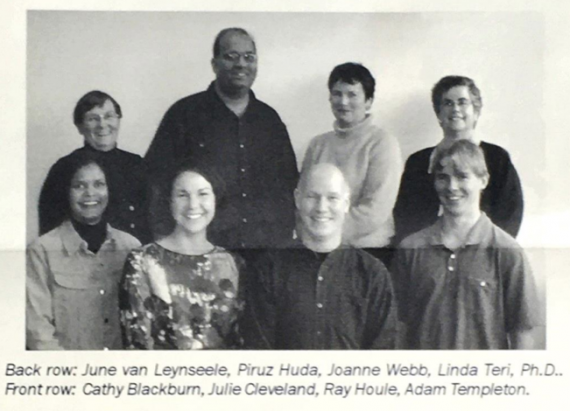
RDAD team, 1990
NIH funding in 1993 made possible the first application of the ABCs to a behavioral intervention designed to reduce physical disability and behavioral problems in patients with Alzheimer’s disease. A group of ADRC-affiliated investigators, including Teri, McCurry, Logsdon, Eric Larson, MD, MPH, and Wayne McCormick, MD, joined together to conduct Reducing Disabilities in Alzheimer’s Disease (RDAD). Rather than focusing on one area of impairment, RDAD tested the first-ever integrated mix of medical, behavioral, and psychosocial interventions, such as exercise. This first study enrolled patients in the Alzheimer’s Disease Patient Registry, a group of Group Health Cooperative members willing to participate in research, created by Larson and Kukull in 1986 to better understand Alzheimer’s disease in the wider community. Over time, RDAD evolved into its present-day form: a home-based exercise program, combined with caregiver training in problem-solving strategies, practical communication, and pleasant events that can improve the lives of cognitively impaired participants and their caregivers.
“I cannot stress how much this program has helped me. It saved our family’s sanity,” an RDAD participant named Tom told the team. Tom had joined the study to get better support and guidance in caring for his father, an African American man living severe dementia and depression. At the end of the intervention, Tom and his father were exercising together four days a week, and his father was now strong enough to get off and on the toilet by himself. Tom reported that using the ABCs helped him solve some of his most vexing caregiving problems. After Tom worked to identify and modify the activators for his father’s habit of undressing at family functions, he was soon able to react calmly, redirect, and assist his father back into clothes.

Susan McCurry, PhD
Studies of RDAD show that the home-based intervention increases physical activity and reduces stress for people living with dementia and their care partners. It has since evolved through various iterations, thanks mostly to funding from the National Institute on Aging, but also state contracts to train Areas Agencies on Aging senior home care staff in Washington, Oregon, and across the country.
In 1999, Teri received a 5-year Pioneer Award from the Alzheimer’s Association to take ABC behavioral management approaches that they had been testing in families living at home and bring them into assisted living settings. The team launched Staff Training in Assisted Living Residencies (STAR), the first program to address the challenges of providing care to residents with dementia in assisted living. “STAR was a game changer,” says Teri. At the time, there were no training or education programs for staff in assisted living care facilities who interacted with people living with dementia, and often depression and anxiety, every day.
As a staff training program, STAR required hands-on work by ADRC team members. Piruz Huda, RN then working as a psychiatric health provider and research study consultant, helped develop the manual and video training components, distributed through the ADRC, used in assisted living facilities. As a STAR trainer, he engaged care staff in role-playing and discussions. “When people describe to me what hasn’t worked, I like to work with them to teach them some simple skills, and find a way that does work,” Huda said at the time in 1999. “To see their appreciation, that they feel better working with the resident, and especially that the resident feels better, is very rewarding.” This and future work resulted in publications that showed STAR improved resident outcomes, reduced dementia-related problems, and improved staff skills and job satisfaction.
Adaptations
Today, many different versions of RDAD, STAR, and STAR-Caregivers (STAR adapted for family caregivers) are part of a group of popular validated non-pharmacological interventions, known collectively as Seattle Protocols, widely adopted in homes, clinics, and facilities throughout the country and world.

“I’ve never felt like I owned these interventions. My goal was always to give it away, to get it into the hands of the people who needed it,” says Teri, who left her role in the ADRC in 2009 to expand RDAD at the UW School of Nursing. She is now focused on helping other researchers to adapt these ABC-based programs for those who may need them the most.
Inspired by the effectiveness of RDAD, Karen I. Fredriksen Goldsen, PhD, Professor at the UW School of Social Work, teamed up with Teri to design and integrate specific components of the intervention to address the unique needs of the aging LGBTQ population and evaluate its effectiveness in an ongoing clinical trial named the Innovations in Dementia Empowerment and Action (IDEA) Study. In this free six-week cognitive behavioral intervention program, a care partner and a person living with dementia are matched up with a coach, who helps both the caregiver and the person experiencing symptoms to develop strategies to solve problems that may arise. The intervention is being offered in Seattle, San Francisco, and Los Angeles.
STAR-Caregivers is undergoing similarly robust expansions and improvements. Currently, UW School of Public Health's Robert Penfold, PhD is working with Teri and McCurry to pilot a less expensive, shorter, virtual version with patients and caregivers at Kaiser Permanente Washington. This effort, STAR Caregivers: Virtual Training and Follow-up, is a NIA-funded clinical trial to improve the behavioral and psychological symptoms of dementia and reduce caregiver burden without the use of anti-psychotic medications. Alongside Penfold, Magaly (Maggie) Ramirez, PhD of the UW School of Public Health is adapting the STAR-Caregivers program to fit the cultural needs of Spanish-speaking Latino family caregivers and developing a mobile app to ensure easy access to the program.
As Teri reflects on the widened landscape of behavioral interventions and culturally-tailored caregiver resources that exist today, she points to a sign of their positive impact. “One encouraging thing I’ve seen over the years is that the idea there’s “nothing you can do” has become less common, while the idea that caregivers can learn helpful behavioral skills has become much more common.”
Despite the relatively increased availability of resources, dementia caregiving will always present some form of the “tangled knot of challenges,” as Teri calls it. “I expect in many ways that the emotional burden for caregivers hasn’t changed from 20 years ago and is probably as intense as ever,” she says. For this reason, the ADRC team continues to honor and build on the long-reaching legacy of the Center’s past foundational work in non-pharmacological interventions. The ADRC, in partnership with the Memory and Brain Wellness Center (MBWC) clinic, serves as a point of referral to the IDEA Study and STAR-Caregivers and spreads the word about these and other opportunities to the general public and ADRC research participants. The MBWC regularly offers a free program, Powerful Tools for Caregivers, as well as many community wellness talks and workshops.
Infused with the MBWC’s emphasis on resilience and mindfulness, these resources help people learn new habits to take care of their own selves while they care for a loved one. At heart, the Center shares Teri’s enduring goal: to support and empower family caregivers to examine their own tangle of physical and emotional challenges, pulling on the loosening threads, until things get a little easier. •
This story has been updated to correctly represent Drs. Peter P. Vitaliano's and Michael V. Vitiello's research.
Images: Shutterstock







