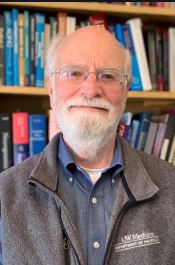
 We are proud to share “Dr. Bird’s Nest – Blog” with the HD Community. Dr. Thomas Bird, founder of the University of Washington HD Center of Excellence, and author of “Can You Help Me? Inside the Turbulent World of Huntington Disease”, has dedicated decades of clinical care and research to Huntington disease. We look forward to hearing from him as he blogs about a variety of Huntington’s disease topics sharing his experiences from 40+ years of caring for individuals with HD.
We are proud to share “Dr. Bird’s Nest – Blog” with the HD Community. Dr. Thomas Bird, founder of the University of Washington HD Center of Excellence, and author of “Can You Help Me? Inside the Turbulent World of Huntington Disease”, has dedicated decades of clinical care and research to Huntington disease. We look forward to hearing from him as he blogs about a variety of Huntington’s disease topics sharing his experiences from 40+ years of caring for individuals with HD.
_____________________________________________________________________________________________________________
February 2024
A Letter from Dr. Bird: 50 Years of the UW Neurogenetics and Huntington’s Disease Clinic
In 1957 Dr Arno Motulsky, Professor of Medicine at the University of Washington’s new Medical School, decided to initiate a clinic devoted to genetic diseases. As a hematologist he was especially interested in hereditary diseases of blood and hemoglobin, but had a prescient vision that genetic factors likely played a role in all medical diseases. With this idea in mind he created the nation’s first Division of Medical Genetics (along with a similar effort at Johns Hopkins). The clinic evaluated and diagnosed any person or family who was thought to have a genetic disease.
In 1973, as a Neurology resident at the UW, I began to visit the Medical Genetics Clinic to offer diagnostic help in evaluating the families with hereditary neurologic diseases. I was amazed to discover that these neurologic disorders were the most common conditions seen in this clinic and that they were incredibly fascinating. The following year (1974) I became a Fellow in Medical Genetics with Dr Motulsky and decided to devote my career to Clinical Neurogenetics.
So in 1974 we began to group the neurological patients together in a weekly clinic and they were seen by me and a more senior Medical Genetics attending physician (such as Motulsky and his colleagues). This was the beginning of the UW Neurogenetics Clinic. I was particularly encouraged in forming this clinic by Dr Motulsky and Dr Judith Hall, a pediatric medical geneticist. The most common disease seen in the clinic was Huntington’s Disease (HD), probably because it was a devastating condition that was not well understood by general physicians in the community and because it was tricky to diagnose based solely on the observation of intermittent involuntary movements. We were ably assisted in these evaluations by Amelia Schultz, a social worker originally trained as an anthropologist at Columbia University, who had developed a special interest in HD.
However, HD was only one of numerous intriguing Neurogenetic diseases seen in the clinic. Other conditions included cerebellar ataxias, Charcot Marie Tooth neuropathy, muscular dystrophies, ALS, epilepsies, mental retardation (as it was called then), neurofibromatosis, Parkinson’s and a variety of dementias. There were no genetic tests, so diagnosis was based almost entirely on family history and physical diagnosis. The clinic became a rich source of material that led to the discovery of numerous genes causing Neurogenetics diseases such as Hereditary Ataxias, Charcot Marie Tooth Neuropathies, Alzheimer’s disease, Frontotemporal Dementia and genetic movement disorders. Important clinical collaborators who attended the clinic included Phillip Chance, Wendy Raskind, Debbie Tsuang, Al LaSpada and Steve Tapscott. International visitors included Anita Harding from Britain, Elsdon Storey from Australia, Mario Cornero from Peru, Ephrat Levy-Lahad from Israel, and Richard Roxborough and Kiri Brickle from New Zealand. Yearly satellite clinics were held in Spokane and Yakima.
Today the UW Neurogenetics Clinic continues to see hundreds of patients and families with hereditary diseases of the nervous system. There are three neurologists (Suman Jayadev, Marie Davis and Anny Lin), a genetics counselor (Mikael Stovarsky), a nurse (Brenda Vicars) and a social worker ( Phaleen Hanson). The clinic includes the HDSA Huntington’s Disease Center of Excellence and a Ataxia Center of Excellence. After all these years, HD remains the most commonly seen disease. Modern genetic testing is heavily used, diagnosis is much more accurate and dozens of “genetic subtypes” of the original disease categories are frequently identified. Neurogenetics continues to be an important player at the forefront of modern medicine.
Thomas D. Bird, MD
Professor (Emeritus), Neurology and Medical Genetics
Previous Blog Posts
Bladder, Bowel and Sexual Problems in Huntington’s Disease
Brenda Vicars, RN, and her team at the University of Washington HD Center have recently published an important study titled “High Prevalence of Concomitant Bladder, Bowel and Sexual Symptoms in Huntington’s Disease”. It has been recognized for many years that persons with HD often have bowel and bladder symptoms, but the frequency and severity of these problems has not been fully characterized. This group of investigators administered a self-reported questionnaire to 48 patients with manifest HD. This group included 26 males and 22 females ranging in age from 22 to 78 (average 48 years). The subjects had had symptoms of HD for an average of 6.8 years ranging from 1 to 22 years. The average CAG repeat expansion size was 44 with a range of 38 to 61. Thus, they studied a fairly typical group of symptomatic patients with HD.
There were numerous important findings from this study. First, a surprisingly high 93% reported symptoms in at least one of the three areas (bladder, bowel or sexual). 87% reported a urinary symptom (incontinence and frequency being most common), 60% reported a bowel problem (constipation being most common), and 56% reported a sexual symptom (particularly decreased sexual activity as the disease progressed). Second, a remarkable 40% reported at least one symptom in all three areas. Hence, concomitant problems in all areas were common. Furthermore, persons with concomitant problems tended to have longer disease duration and worsening total functional capacity scores.
This study emphasizes that HD affects all parts of the nervous system, not only cognitive and behavioral regions, but also the autonomic nervous system and spinal cord. All these areas can influence control of bowel, bladder and sexual function. These pelvic organ systems are very important players in arriving at quality of life. Their dysfunction can seriously impair our activities of daily living. The study authors rightly conclude that “it is important for health care providers to recognize these symptoms and account for them in the overall treatment and management of patients with HD as they would other functional deficits. Many patients will present with a combination of urinary, bowel and sexual dysfunction which should be addressed in a holistic manner.”
Brenda Vicars, RN was able to recently discuss this important topic with Lauren Holder, Producer, Help 4 HD International on her radio podcast titled “Bladder, bowel and sexual dysfunction”. The interview can be heard here: www.help4hd.org/podcast/episode/2defdb80/bladder-bowel-and-sexual-dysfunction
The study publication can be read online at: https://doi.org/10.3390/jpm11080714
Best wishes and be well,
![]()
A year ago, in October of 2020, the topic of this blog was the danger of falls in HD and the occurrence of head trauma followed by bleeding between the brain and skull (known as subdural hematoma). Over the past two years we have collected and analyzed our experiences with this unfortunate outcome of falling and recently published our results in the Journal of Huntington’s Disease. (You can find the details of this report on the internet.) Dr Marie Davis at the UW is the first author of this report and we collaborated with Dr Lauren Talman at OHSU in Portland and Dr Vicki Wheelock at UC Davis in Sacramento. Those three HD Centers were able to identify 25 persons with HD who had experienced one or more subdural hematomas. The fact we could find 25 such cases shows that this is not a rare occurrence, but it is not often mentioned in the Huntington’s literature. For that reason it’s worth reviewing some of the details here.
There were 16 females and 9 males ranging in age from 43 to 89 at the time of the subdural (the average being 60 years). Most of the patients had moderately severe chorea and experienced a fall, often while walking on uneven ground. One person fell while skiing, another while entering a bus and another while descending stairs. Surprisingly, four patients had no known fall or head trauma and probably hit their head unnoticed against a wall or furniture because of uncontrolled head movements. Twelve persons had bleeding on both sides of the head and 5 had a recurrence of the subdural.
The seriousness of subdural hematoma is shown by the fact that sixteeen patients required surgery, meaning a neurosurgeon had to drill a hole in the skull and remove the blood. Such a hospitalization can cost $50,000 or more. One person was left with a seizure disorder as a result of the head trauma and required lifelong anti-seizure medication. Furthermore, two persons died as a direct result of the trauma.
Persons with HD are at high risk for falling because of uncontrolled movements, impulsivity and poor judgment. They are at increased risk for a subdural hematoma because of underlying brain atrophy. The key is for the patient and caregivers to focus on preventing falls and thus preventing head trauma: a perfect example of “an ounce of prevention is worth a pound of cure”!
Best wishes and be well,
![]()
In the early years of this century the Huntington’s Disease Society of America (HDSA) decided to direct a substantial portion of the funds it raised to establishing clinical centers of excellence. Their purpose would be to evaluate and manage persons with HD by connecting them to physicians and health care providers who were especially knowledgable and experienced in the field of HD. This was particularly important because so few physicians nationwide had any experience dealing with HD.
The key idea was for each center to have a multidisciplinary team that could attend to all aspects of HD care. The core personnel consisted of a physician (usually a neurologist) and a social worker, both experienced with HD, and a panel of specialists in a variety of medical areas such as psychiatry, physical therapy, occupational therapy, speech therapy, nursing and genetic counseling. The HD patient and his or her family could find a team of specialists who understood and were experienced in managing all the multifaceted problems associated with HD. The centers would also be involved with education and research, but patient and family evaluation and management remain the core functions.
In the early years there were only a handful of centers, but by 2015 there were 20. In the past five years fund raising by HDSA has been very successful and the commitment to the Centers of Excellence (COE) has been strong and unwavering. In the past year $1,750,000 has been directed to an amazing 50 COE’s. There are now centers from New England to the Pacific Northwest, Florida to California and Texas to North Dakota. Thousands of patients are getting focused, top notch care. The program has been a stunning success. Nevertheless, the demand still exceeds the resources. If the fundraising can grow, so will program.
The University of Washington has been fortunate to have had an HDSA COE for nearly 20 years. The COE Director is Dr Suman Jayadev and her amazing and dedicated team includes Drs Marie Davis and Anny Lin (Movement Disorder specialists), Susan Reynolds ( Social Worker) and Brenda Vicars (Nurse). These professionals really know and understand HD and can bring years of experience to bear on what are often very complicated problems. They are there to serve the HD community. If you have an HD question or problem, give them a call.
Best wishes and be well,
![]()
Clinic Scheduling
Debbie Olson, Program Support Supervisor
206-598-3983 | olsondl@uw.edu
Social Worker
Susan Reynolds, LICSW
206-598-4394 | reynos2@uw.edu
Registered Nurse
Brenda Vicars, RN
206-598-8753 | bvicars@uw.edu
Amelia Susman Schultz was born in Brooklyn, New York in 1915, during the time of social turmoil famously captured by Betty Smith in “A Tree Grows in Brooklyn”. There was absolutely no reason to suspect that Amelia would become a pioneer social worker in the fields of Medical Genetics and Huntington’s Disease, since neither field existed at that time, but that is how things turned out. Her father was an accountant and her grandparents ran a bakery. Her younger sister, Harriet, was developmentally disabled with life-long struggles and would have an important influence on Amelia’s later choice of career in the healthcare field. Amelia graduated from Brooklyn College in 1936 during the depths of the Depression with assistance from the Federal Works Progress Administration (WPA). She was determined to do graduate work at Columbia University and was interested in both Psychology and Linguistics. When told the Psychology department did not accept women or Jews she applied to Anthropology and was accepted.
In the Anthropology department at Columbia Amelia was mentored by, and rubbed elbows with, international leaders in the field including Franz Boas, Ruth Benedict, Margaret Mead, and Ralph Linton1. Boas was nearing the end of his career as the founder of American Anthropology. He was known for his tolerance and his emphasis on cultural interactions but took a dim view of anthropologists’ frequent emphasis on race. For example, much to the distress of proponents of race theories, he pointed out that human head size and shape was more related to environmental factors than to ethnic background. Looking back on those days Amelia says “Boas was the greatest man I ever knew”. She also had a high regard for Ruth Benedict who helped her with her studies. She says that Margaret Mead was her bête noir. She considered Mead wordy, unreliable and egocentric. Linton was also to eventually disappoint her.
Amelia pursued her linguistic interests by traveling to Seattle and Prince Rupert, British Columbia to study the language of the Tsimshian Indians. However, this project ended when she was asked by Linton to contribute a chapter to a forthcoming book on acculturation of eight Indian tribes. She was assigned the tribes in the Round Valley Reservation of Mendocino County, California, north of San Francisco. She traveled to the area, immersed herself in the experiences of the tribes and in their contact with whites. She composed what was supposed to be her PhD dissertation. Her chapter for Linton’s book unstintingly described the harsh, violent and racist behavior of the white Americans toward the Native Americans. Amelia was frankly appalled by what she saw and learned. She documented the fraud, abuse and murder perpetrated by the settlers, miners, and ranchers with little or no provocation, referring to this as negative acculturation. She returned to Columbia pleased with her freshly written dissertation. Several weeks later Professor Linton had Ruth Benedict inform Amelia that the title of the upcoming book was being changed to “Acculturation of Seven Indian Tribes” and her dissertation was not being accepted as a chapter 2. Dissertations had to be published to count for the PhD degree, so she would also not be receiving her degree. Amelia never received any direct comments about what she had actually written, but was led to believe that the department and/or the publisher wanted to avoid a possible lawsuit from the California ranchers. Her chapter was not politically correct and even seemed a bit “un-American”. Acculturation was supposed to be working successfully and this was evidence that it was not.
Rather than giving up when faced with this unexpected and stunning reversal, Amelia scrambled to quickly find another dissertation project. She proved extremely resourceful. She was able to write a complicated and academically sound paper on the linguistics of the Winnebago language by studying a small family of Indians from this tribe who happened to be performing in a carnival in Atlantic City. She turned in her second dissertation and waited for the results.
Meanwhile, our country was being consumed by World War II. Feeling patriotic, and needing a job and income, Amelia joined the Army and became a WAC (Women’s Army Corps). Her experience in the Army was to change her life and set her on a new career path. She was assigned to Mason General Hospital in Deer Park, Long Island. The War Department had taken over several of the buildings and also part of the campus of the huge Pilgrim State Psychiatric Hospital (an insane asylum) and turned these into a facility for rehabilitating soldiers disabled by “shellshock” or “battle fatigue”, what we now call PTSD. Amelia counseled the soldiers, dealt with their families, and helped them find employment after discharge. Looking back on the experience she realized that she was becoming a self-trained psychiatric social worker. While stationed at the hospital she also received her PhD diploma in the mail without comment and her “second” dissertation was published by Columbia University Press in 1943 3.
Following the war Amelia moved to Seattle. During her Native American studies she had fallen in love with the Pacific Northwest, not only the forests and mountains, but the ability to avoid the hot, humid summers of the East Coast. Over the next several years she spent time traveling and took a number of part time jobs as a social worker.
In that same time period the University of Washington inaugurated its new School of Medicine and the first class graduated in 1950. The school had all the excitement and energy of a fresh academic enterprise. In 1960 Amelia applied for and was accepted as the first social worker for two new components of the UW Medical School. Part of the week she was the social worker for the CRC (Clinical Research Center) and on the other days she was assigned to the newly established Medical Genetics Clinic. In 1957 Dr. Arno Motulsky had started one of the first clinical Medical Genetics programs in the nation. Thus, without intending to do so, Amelia became one of the first, if not the first, social worker for a Medical Genetics clinic. She was a pioneer.

In the early days the clinic mostly saw families with hematological disorders (Dr. Motulsky’s specialty), mental retardation, especially Down syndrome, and muscular dystrophy. Over time, however, Amelia began to see families with Huntington’s disease. She had only heard of the disease from some of her psychiatric colleagues, but was now faced with the manifestations and implications of HD. The social work needs of the families were voluminous and her practice slowly became focused on HD. The clinic charts of HD families began to fill with pages of notes by Amelia, typed on her portable Smith Corona, documenting their unemployment, financial turmoil, scrapes with the legal system and need for nursing homes. She made field trips to Western State Psychiatric Hospital to visit patients who had been committed there. When the local HD families banded together to form a support group Amelia became the liaison with the UW clinic. She formed a two person team with another member of the support group whose husband had HD and they gave in-service sessions at nursing homes and hospitals throughout western Washington. Her teammate’s husband died of HD and all three of her adult children developed the disease. That woman eventually committed suicide creating yet another heavy load for Amelia to bear. Amelia formally retired in 1977 after 17 years as the Clinic social worker, but for another decade she remained the “go to” person for HD problems. She became friends with Marjorie Guthrie, Woody’s wife, on Marjorie’s trips to the West Coast. In 1977 Amelia helped Marjorie organize a commission on Huntington’s Disease in Seattle during a national investigation of the disease sponsored by NIH. Marjorie had founded the Committee to Combat Huntington Disease, an early precursor of the Huntington Disease Society of America.
Ironically, with the support of her many friends, Amelia’s dissertation on the Acculturation of the Round Valley Indian Tribes that had been turned down by Columbia in 1940 was published by the University of California, Berkley in 1976 4 . A review in the California Journal of Anthropology noted that her paper had simply been ahead of its time and was too controversial for the 1930s, even though its observations were accurate, poignant and damning. She witnessed and documented the aftermath of what, more than 70 years later, Benjamin Madley would describe as the “California Indian Catastrophe” 5.
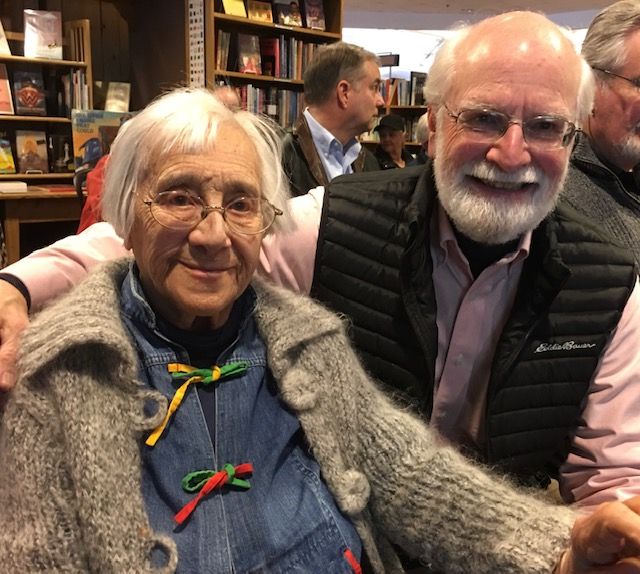 During my training in Neurology and Medical Genetics Amelia Susman Schultz first introduced me to the world of Huntington’s Disease. In December 2014, at age 99, I interviewed her for my upcoming book about HD which was dedicated to her 6. She was sharp and accurate in her recollections and had not lost her opinions or sense of humor. She died on April 23, 2021, just a few weeks short of her 106th birthday, after living a long, fascinating and productive life.
During my training in Neurology and Medical Genetics Amelia Susman Schultz first introduced me to the world of Huntington’s Disease. In December 2014, at age 99, I interviewed her for my upcoming book about HD which was dedicated to her 6. She was sharp and accurate in her recollections and had not lost her opinions or sense of humor. She died on April 23, 2021, just a few weeks short of her 106th birthday, after living a long, fascinating and productive life.
Thank you Amelia!
![]()
- King, Charles, Gods of the Upper Air: How a Circle of Renegade Anthropologists Reinvented Race, Sex and Gender in the 20th Century, Doubleday, New York, 2019.
- Linton, R. (Editor), Acculturation in Seven American Indian Tribes, Appleton-Century, NY, 1940.
- Susman, Amelia, The Accentual System of Winnebago, Columbia University Press, NY, 1943.
- Susman, Amelia, The Round Valley Indians of California, University of California – Berkley Archeological Research Facility Contributions, N. 31, 1976.
- Madley, Benjamin, An American Genocide: The United States and the California Indian Catastrophe 1846-1873, Yale University Press, 2016.
- Bird, Thomas, Can You Help Me? Inside the Turbulent World of Huntington Disease, Oxford University Press, New York, 2019.
Two announcements in the past few days have greatly disappointed the HD Community. First, Roche announced they had stopped their attempt at an ASO (anti-sense oligonucelotide) treatment of HD. The Independent Data Monitoring Committee (IDMC) requested the halt for reasons that have not yet been explained. IDMC’s have a primary responsibility for monitoring patient welfare, so there must be a good reason. More information will soon be available.
Second, the WAVE study, a somewhat different ASO trial, was also stopped. The reason for the halt was a lack of significant reduction in huntington protein which was an important biologic measure of the study’s success.
We need to put these major negative announcements into perspective. It is worth recalling that the vast majority of clinical trials in medicine are “failures”. That is, they never advance to a treatment that receives FDA approval. A perfect example is the last decade of attempts to treat Alzheimer’s disease (AD). AD is another neurodegenerative brain disease for which there is a considerable amount of understanding about the underlying biochemical abnormality. And yet numerous biologically reasonable approaches to treat these abnormalities have failed. This includes failure to effectively treat persons with an autosomal dominant genetic form of AD with many similarities to HD.
Also, it is instructive to remember that the treatment approaches to Alzheimer’s seem to have worked quite well in mouse models of AD. We learn over and over again that mice are not humans. There are immense differences between the two.
Furthermore, optimism about treating genetic neurologic diseases received a big boost a few years ago with successful trials to treat spinal muscular atrophy (SMA). These were trials directed at treating the specific genetic defect using either spinal fluid or intravenous approaches. However, the genetic treatment of SMA differs from HD in many ways. Differences include the inheritance pattern (autosomal recessive in SMA), the molecular genetic defect (not a repeat expansion in SMA), the age of onset (infancy), the age at which treatment is started (infancy) and types of nerve cells attacked by the disease (probably restricted to motor neurons in SMA versus many different nerve cell types in HD). Thus, success in SMA treatment trials did not necessarily suggest success in HD.
Nevertheless, there is still good news. For example, there are several additional treatment approaches to HD still in the clinical trial pipeline. We should cautiously look forward to their advancement. Also, WAVE has not given up. They plan a further study using a newer and hopefully better chemical to attack the HD mutation. So, there are always ups and downs, but science marches forward. There is too much known about the biology of HD to stop pursuing attempts to stop the progression or even reverse the disease.
Perhaps the words of our poet laureate, Amanda Gorman, are most appropriate:
“The new dawn blooms as we face it.
There is always hope,
If we are brave enough to see it,
If we are brave enough to be it.”
Be careful. Stay safe.
![]()
From time to time we have seen patients with very obvious signs of HD who completely refuse to believe they have the disease. More commonly, some persons with HD recognize they have the disease, but cannot see they are affected by some important aspect of it. It used to be said these people were in “denial”, but it has become clear that they actually are not aware of their disability. This is referred to as “lack of awareness” and it is a relatively common occurrence in HD.
The formal medical term for lack of awareness is “anosognosia” which means “a lack of ability to perceive the realities of one’s own condition.” It is a person’s inability to recognize that they have a trait or condition that matches up with their symptoms or diagnosis. The manifestations are obvious to an observer, but are underestimated or not even acknowledged by the affected person. The condition is clearly the result of a dysfunctional brain, but the exact physiology is not understood.
Lack of awareness can be relatively harmless or it can produce havoc in trying to manage the individual’s daily activities. For example, a person can be unaware of involuntary movements, but they may not be causing any particular problems. The person is getting along quite well with minor incoordination. On the other hand, the movements may create serious problems with driving ability creating a real danger, but the patient sees no difficulty and continues to drive. This can end badly and needs to be addressed.
There may be a lack of awareness of impaired judgement that can lead to inappropriate spending, overdrawn checking accounts and out of control credit card debt. The individual may be making serious mistakes at work and have no idea that he or she is about to lose their job. He may be angry at his supervisor for pointing out mistakes that he does not view as mistakes.
This phenomenon frequently leads to disruption of medical care. The unaware patient sees no reason to attend clinic, to see a doctor or to take “unnecessary” medication. He or she refuses help because “there is nothing wrong”.
Dealing with lack of awareness can be a major challenge for care takers. The autonomy and independence of the patient need to be respected. It is usually counterproductive to “argue” with the patient, because the lack of awareness is not conscious denial, but an actual inability to appreciate reality. The goals are to keep the person safe and calm. Direct action is sometimes necessary, such as denying use of a car when driving has become dangerous. Negotiations with the workplace may be needed when occupational requirements can no longer be met. We have seen instances where explaining the disease to an employer has resulted in a medical retirement instead of firing for incompetence.
Sometimes the individual will agree to see the doctor about back pain or a general checkup or agree to take medication for a specific non-threatening symptom.
Overall, it is important for caretakers to recognize when lack of awareness is playing a role in the person’s behavior. This can allow for avoidance of confrontations and more reasonable approaches to reach the desired goal. A successful strategy requires patience, persistence and sometimes imagination, but can be worth the effort.
Be careful. Stay safe.
![]()
The first symptoms of Huntington’s Disease can be quite subtle and difficult to detect. Physicians having extensive experience with HD get very astute at noticing early signs of chorea such as brief but persistent involuntary movements. These may not be noticed even by the patient or family members. Taking these early signs into consideration it has traditionally been said that HD usually “starts” in midlife (meaning 35 to 55 years) and slowly progresses until death 15 to 20 years later. It is well known that there are outliers with onset at an earlier (juvenile) or later (elderly) age.
However, these age of onset guidelines are predicated on motor symptoms or signs such as involuntary movements, especially chorea. It became clear that if one took into consideration behavioral changes, then the onset might be much earlier. Personality changes can occur in some persons many years prior to abnormal movements. It is more difficult to know for certain if a personality change is actually due to HD, but it certainly can be and may be the first sign. So someone can have a behavioral
change in his or her 30’s and not develop chorea until the 40’s, but it could be said that the HD “started” in the 30’s.
The next development in this theme was introduced by brain imaging techniques such as CAT and MRI scans. Taking persons who had inherited the HD genetic mutation, but had no symptoms, researchers could show that there were areas of brain atrophy that preceded symptoms by as much as 10 years (or even more). So physical brain changes were starting long before symptoms. Furthermore, brain scans in children who carried the mutation showed brain changes even before adolescence, even though the children were functioning perfectly normally.
The latest development was reported last year by researchers in France. Under the microscope they examined the brains of human fetuses which carried the HD mutation. They found that there were clear abnormalities in the developing cerebral cortex. They found an improper migration and mislocalization of nerve cells and evidence of nerves cells that had not developed properly.
Thus, it can be said that biologically HD “starts” at conception. This should not be a surprise, given that this is a genetic disease and the cells with the HD mutation are there from the beginning. Fortunately, the brain is able to compensate for these subtle changes for many decades. The good news is that there seems to be an angle of repose or tipping point at which symptoms begin that is not reached for many years.
Of course numerous questions remain. Why is that tipping point age ten years in some persons and age 75 in others? The CAG expansion size explains some, but not all of this phenomenon. And how early should treatments begin to be most effective: at the time of early symptoms or years earlier? These are very important questions are are under active and intense investigation. The answers will add fascinating new pieces to the HD puzzle.
Be careful. Stay safe.
![]()
Sleep is a critical aspect of human behavior. Too little sleep can create chaos in our waking lives. Too much sleep interferes with our ability to get things done. We all need about 8 hours of sleep each night for proper daytime functioning. Some people naturally get along with less and some need more, but 8 hours is the ideal for almost everyone.
Problems with sleep are common in Huntington Disease. The most frequent sleep problem is insomnia manifesting as trouble falling asleep, or early awakening, or hardly sleeping at all. This can be associated with pacing or agitation at night which is unsettling to the individual and can be very disturbing to caretakers and family members. One can also experience a shift in sleep patterns such that the individual is awake at night and then sleeps much of the day. Inability to fall asleep at night associated with confusion and wandering is often called “sundowning”. At least 40 to 50% of HD patients describe one or more of these sleep problems and consider them some of their most serious life disrupters. And HD is not alone: sleep disturbance is also common in other neurological diseases such as Alzheimer’s and Parkinson’s. (In fact, there is a very rare genetic brain disease called Familial Fatal Insomnia.)
A frequent question is what happens to involuntary movements during sleep? It used to be stated that chorea always disappeared during sleep. More recent studies have shown that although that is often the case, sometimes the movements continue and may even interrupt the sleep pattern.
Several things can worsen sleep problems. Depression and anxiety go hand in hand with insomnia and all three are common in HD. Likewise, both caffeine and alcohol make it harder to fall asleep and stay asleep. And smoking in bed is forbidden! Not only can it disturb sleep but it is a serious and very dangerous fire hazard.
Treating sleep disorders in HD is not easy. Avoiding caffeine, alcohol and smoking is a good start. Daytime exercise such as frequent walks can be beneficial. If there is associated depression, then an antidepressant medication may help. Many medications used to induce sleep have unwanted side effects such as prolonged lethargy during wakefulness, addiction potential, loss of effectiveness with prolonged use and nightmares. Over the counter melatonin may help and has the fewest side effects. In fact there is some research evidence for reduced melatonin levels in HD. Stimulants are rarely helpful for daytime sleepiness and may produce unwanted agitation.
If you or a family member has these sleep problems, try to get into a daily activity routine and use some of the tips mentioned above. The goal is for everyone to get sufficient sleep. Don’t be afraid to ask for help. Good luck and sweet dreams.
(If you are interested in more details about HD and Sleep, the following is a good up-to-date review: Herzog-Krzywoszanska, “Sleep Disorders in Huntington’s Disease”, Frontiers in Psychiatry, 2019, 10:221.)
Be careful. Stay safe.
![]()
For a disease known for its hyperactive movements it might come as a bit of a surprise to learn that apathy is a common symptom in Huntington’s Disease. Persons with HD often seem to lack energy and initiative. They have no “get up and go”. They may become the proverbial couch potato. I can recall a patient who spent all day watching television and did not remember anything he had seen. Another patient spent hours at the kitchen table reading the newspaper with little comprehension. This disinterested, sedentary lifestyle can be especially frustrating to family, friends and caretakers. What do we know about this common symptom of HD?
Several studies have investigated the association of apathy with HD and drawn a number of conclusions. Apathy is quite common in HD, occurring in 30 to 70% of patients depending on the study and the stage of disease. It is often divided into 3 types: Emotional apathy causes emotional blunting and lack of interest in previously motivating activities. Cognitive apathy results in poor planning, poor organization and trouble shifting attention. Motor or Activation apathy refers to a reduction in self-generated physical activity. All three types can be seen in HD.
Apathy can be confused with depression which is also common in HD. However, several studies have shown that they are not the same and do not necessarily occur together. It has been shown that depression occurs with about the same frequency in all stages of HD, but apathy actually increases as the disease progresses. This strongly suggests that apathy is a symptom directly caused by the degenerative process in the brain, presumably a deterioration of the connections between the caudate and the prefrontal areas. This also fits with the finding that apathy is common in other degenerative brain diseases such as Parkinson’s and Alzheimer’s.
Treatment of apathy is difficult and often not very successful, but behavioral therapy approaches are worth trying. For example, taking the individual for walks or car rides can produce a change of environment that may be stimulating. Encouraging them to get engaged in hobbies or activities that previously interested them may help. Stimulant drugs rarely work and sometimes result in exchanging apathy for even worse and unwanted agitation. Frequently letting the subject be quiet and uninvolved works the best and they seem to be perfectly satisfied. That was the case with the two patients I mentioned at the beginning. The apathy sometimes seems to be more frustrating for the caretaker than for the patient. Finding the right balance takes time, but is often achievable.
Be careful. Stay safe.
![]()
George Huntington was born in 1850 in the town of East Hampton far out on the South Shore of Long Island. His father and grandfather had both been family doctors in this town. George followed in their footsteps and graduated from Columbia’s College of Physicians and Surgeons in 1870. He then moved to Ohio to begin his practice and needed to present a paper before his new county medical society. What topic should he choose?
In a memoir written later in life Huntington recalled as young boy driving with his father through a wooded road in East Hampton. They came upon a mother and her daughter who were well known to his father. He remembered them as “cadaverous, bowing, twisting and grimacing.” He said he “stared in wonderment” and thus began his education as a physician. This experience must have come to his mind as he was choosing a presentation for his new medical society in Ohio. The title of his topic was “On Chorea” and it was published in 1872 in the Philadelphia Medical and Surgical Register. So at age 22 he had written what was to become known as one of the finest brief descriptions ever published of a neurological disease.
Huntington’s “On Chorea” is only 4 pages. The first half deals with a different condition that is known as Sydenham’s Chorea. Huntington may have seen cases of this during his medical school experience. It is a self-limited movement disorder that occurs in childhood and we now know to be related to rheumatic fever. He reviews the typical presentation of this disease and mentions several hundred cases that had been previously reported. Nothing new here.
Then on the third page of his paper Huntington switches gears and says “And now I wish to draw your attention more particularly to a form of the disease (meaning chorea) which exists, so far as I know, almost exclusively on the east end of Long Island. It is peculiar in itself and seems to obey certain fixed laws.” He then proceeds to describe the details of the family his father and grandfather had cared for over many decades. Remember, George himself had not practiced in his hometown and was only describing what he had noticed growing up as a boy and observing the family members as they wandered in the village and were seen by his father.
Huntington states that this disease has “three marked peculiarities: 1. Its hereditary nature. 2. A tendency to insanity and suicide. 3. Its manifesting itself as a grave disease only in adulthood.”
In terms of heredity he points out that either parent can have the disease and it is passed on to children without skipping a generation. He notes that this is different from the so-called hereditary nature of tuberculosis or syphilis which often skip generations. He then specifically says that if a child survives into advanced adulthood without developing the disease, in that branch of the family “the thread is broken”, the disease “has yielded its claims and never again regains them.” He had nicely described autosomal dominant inheritance three decades before the medical world became aware of this biological phenomenon. (He had observed that men were more often affected than women in his local family, but this turned out not to be the case in larger population studies.)
In terms of insanity he mentions that the “mind becomes more or less impaired”. He describes inappropriate social behavior (“never let an opportunity to flirt with a girl go past”) and a tendency to suicide.
Huntington mentions the adult onset of the disease as being usually in the 30’s in order to clearly distinguish it from the sporadic childhood form of chorea. He notes that the spasmodic movements are mild at first, but gradually become severe affecting the entire body and “presents a spectacle which is anything but pleasing to witness”. “I have never known a recovery or even an amelioration of symptoms” and “when once it begins it clings to the bitter end.” (This also makes the disease completely different from childhood chorea.) He notes that family members often view the condition “with a kind of horror” and “that medical advice is seldom sought”.
Huntington ends his paper saying “I have drawn your attention to this form of chorea gentlemen, not that I consider it of any great practical importance to you, but merely as a medical curiosity, and as such it may have some interest”. Little did he know that he had just succinctly described one of the most important neurogenetic diseases of all time to which his name would be forever attached!
As a footnote it has been mentioned that this disease may have been briefly described two or three times before Huntington, but never in such accurate detail, and many so-called earlier descriptions were more likely of Sydenham’s Childhood Chorea. Also, George Huntington moved back to New York State in 1874, but took up practice not in East Hampton but in Duchess County along the Hudson River north of Manhattan. He never published another medical paper.
Alice Wexler has written an excellent and thorough account of this first family with HD in which she relates the story of Phoebe Hedges who was affected with the disease and ended her life as “the woman who walked into the sea”. Our friend David Johnson discovered that Phoebe’s grandson, Hiram, travelled the Oregon Trail in 1850 (the year of George Huntington’s birth) and one of his descendants died in the Oregon State Mental Hospital in Salem. This is undoubtedly the first introduction of HD into the Pacific Northwest.
(Wexler, Alice, “The Woman Who Walked Into the Sea”, Yale Press, 2008.)
For nearly 100 years Huntington’s Disease was known as Huntington’s Chorea. The term chorea emphasized the dance-like movements that were often (but not always) a prominent part of the disease. When these involuntary movements involve walking they produce an irregular, poorly coordinated gait that can result in falls. The falls, of course, can lead to trauma. The trauma can be mild, like a stubbed toe or sprained ankle, or severe, like a broken arm or fractured hip. This severe trauma can lead to emergency room visits with the associated expenses and sometimes hospitalization with even more expensive surgery.
An under-recognized result of falls in HD is serious head trauma. This head trauma can cause bleeding into the space between the skull and brain called a subdural hematoma. The resulting symptoms depend on the size of the hematoma and can include headache, dizziness, confusion or lethargy. The diagnosis requires a CAT scan or MRI of the head. Sometimes the hematoma can simply be followed by the healthcare team and will slowly resolve itself. Unfortunately, if it is enlarging or causing pressure on the brain, it may require emergent surgical removal by a neurosurgeon.
Our HD Center at the University of Washington has been collecting information on our patients who have developed subdural hematoma along with our colleagues at Oregon Health Sciences University in Portland and UC Davis in Sacramento. We are reviewing nearly 20 such cases. There are both men and women in the study and a wide range of ages from 40’s to 80’s. The most common characteristic preceding the fall was the presence of considerable chorea. Surgical removal was required in several cases and there were two deaths, so this is not a benign occurrence. Interestingly, at least two persons had no history of any fall. They probably injured their heads from sudden jerking neck movements causing the head to hit the wall or furniture.
There are a variety of medications that can ameliorate chorea, but nothing can completely eliminate it. The bottom line is that individuals with HD need to be especially cautious when walking, especially on uneven ground or broken sidewalks and always use railings on stairs. With onset of poor coordination assessment by a physical therapist is a good idea. Canes and walkers can be very useful and a wheelchair is much better than a subdural hematoma!
Be careful. Stay safe.
![]()
September 2020 – Psychosis in Huntington’s Disease
The occurrence of psychosis in persons with HD gets relatively little attention, but when it occurs it can be severely debilitating. Thus, it deserves thoughtful discussion.
It is often stated that psychotic features are seen in about 5 to 10% of individuals with HD, but a recent study by Dr. Ashwin Jaini and colleagues at Northwestern University in Chicago, found a frequency of 13% in nearly 8,000 participants with HD in the ENROLL-HD database. This might even be an underestimate of the actual frequency because persons with marked psychosis are less likely to take part in ENROLL-HD. Given this remarkable frequency we should review some of the details regarding this association.
Psychosis is usually described as a serious detachment from reality. Persons with psychosis often have hallucinations or delusions or both. In addition their speech may be nonsensical or incoherent and they may be very withdrawn socially.
The hallucinations can be visual or auditory, but usually auditory. They may hear strange people talking to them or even giving them peculiar instructions. They may be quite bothered by these voices, but unable to stop them.
The delusions can be uncomfortable, even frightening and often have an element of paranoia. We had one patient with HD who thought strangers were after him and spying on him so he covered all his windows with aluminum foil. Another individual thought the devil was telling him to injure his friends and relatives, a combination of auditory hallucinations and delusion. Others erroneously thought family members or caregivers were poisoning them. These kinds of symptoms are impressively described in the movie “A Beautiful Mind” based on the true story of John Nash who suffered from paranoid schizophrenia (and also won a Nobel Prize in Economics!).
The treatment of psychosis is difficult because the individual believes the symptoms to be very real and cannot be talked out of them. Antipsychotic medications can be quite helpful in that they may help the person feel more comfortable and make the hallucinations and delusions less threatening. There can be definite improvement in seriously disabling behavior. However, the drugs do not make the symptoms disappear and they have side effects that can include lethargy, general slowness, weight gain, stiff muscles and abnormal movements. The treatment is always a trade off between helpful benefits and undesirable side effects. Usually one can start with a low dose and increase as necessary.
The reasons why persons with HD develop psychosis are mostly unknown. The association suggests similarities between HD and schizophrenia and another degenerative brain disease called frontotemporal dementia (FTD). The symptoms are likely to be the result of nerve cell dysfunction in the frontal lobes and striatal system (caudate and putamen) of the brain, which are abnormal in all three of these diseases. Clearly much more research is required to understand these disturbing symptoms and discover better treatments.
![]()
August 2020 – What Troubles You the Most?
Huntington’s Disease has a tremendous variety of symptoms and problems that can appear in any particular person at any particular time: chorea, dystonia, ataxia, depression, anxiety, anger, delusions, mania, poor temper control, confusion, impaired judgement and social embarrassment (to name just a few). If you ask someone with HD “What troubles you the most?” what do you think they would say?
A group of investigators decided to ask HD subjects that exact question. They recently reported the answers they received in a publication in the journal NEUROLOGY (2020, 94:823). Let’s review what they discovered.
The study was done by Alistair Glidden and his colleagues at the University of Rochester, Emory University in Atlanta and the University of Michigan. They first performed detailed interviews with 20 persons with HD and 20 caregivers to determine what were mentioned as their most important and troublesome symptoms. From these interviews they devised a 216 item symptom questionnaire which covered 15 symptomatic themes. The asked both how often do you experience each symptom and how much does each symptom impact your life? The questionnaire was then given to 96 persons with symptomatic HD, 60 with prodromal HD and 233 caregivers. The subjects were 95% white, predominantly female (69%), mostly high school or college educated and with an average age of 44 years (range 20-71).
Despite HD being typically associated with abnormal movements and coordination problems, “emotional issues” was the most frequently experienced symptomatic theme and “difficulty thinking” was the theme having the greatest impact on their lives. Looking more closely at the details the most common symptoms were fear of disease progression, frustration, anxiety, problems concentrating, burden of thinking about the future and being tired or fatigued. Communication difficulties and trouble dealing with social situations were also common. The symptoms having the highest average impact on their lives were impaired sexual function, inability to drive a car, impaired sleep and fear that one’s ability to think would worsen.
In my own experience the results of this study ring true. The responses seem to be a fairly accurate analysis of what concerns the typical person with HD. In fact, given our knowledge that many persons with HD often have a “lack of awareness” about their problems, the subjects in this study seem to have been quite frank and insightful. Of course, it is likely that some persons with severe or advanced HD would not have been able to complete a 216 item questionnaire and thus were missed in the study.
It turned out that caregivers generally agreed with the symptomatic subjects about which problems were most prevalent. However, caregivers consistently reported thinking that the symptoms had a greater impact on the individual’s life. This is a common theme in many diseases: caregivers perceive more disability in an individual than the individual does in himself or herself.
So there you have it. Persons with HD are most troubled about emotional and thinking problems, difficulty in social situations and worry about the future. They are frustrated by sexual dysfunction, sleep problems and inability to drive. Caregivers and health care providers need to listen to the patients and keep these observations in mind when interacting with the HD community.
![]()
July 2020 – What Is Juvenile Huntington’s Disease?
Last month we discussed late onset HD. Sad, but true, children can also develop this disease. So now let’s look at the other end of the age spectrum.
Juvenile HD is defined as those persons who have their first symptoms before the age of 20.
This represents about 10% of all HD. Even more unusual, about 2% have onset before age 10. Over many decades we have seen about 30 to 40 children with HD at the University of Washington.
In addition to age there are several things about juvenile HD that make it different from the more common adult form. For example, chorea is frequently not seen in juvenile HD. It is more common to have clumsiness, poor coordination and stiff muscles. These symptoms are often combined with deterioration in school performance. Because chorea is uncommon and the early symptoms are subtle, the disease often goes unrecognized until the disability is obvious.
Like adult HD, juvenile HD is progressive, but unfortunately the progression is more rapid. The disease typically lasts about 8 years in juvenile HD compared with 15 to 20 years in the adult variety. Also seizures are fairly common when the onset is before age 10, whereas seizures are rare in adult disease.
The early onset of HD is closely correlated with especially large CAG repeat expansions in the HD gene. Children with juvenile HD usually have CAG repeat sizes larger than 60, frequently larger than 80, and sometimes 100 or more. This is in contrast to adult disease in which the CAG size is typically between 40 and 50.
Parents in families with HD often ask if they can do genetic testing on their children to discover whether or not they have inherited the mutation. In general this is discouraged. This is because a positive test in the usual range (40-50 CAG) might not be associated with actual symptoms for many decades. Meanwhile the child would be “labeled” as having the HD mutation and might well be treated differently by parents, teachers, peers and others in the community (so called “self-fulfilling prophesy”). Furthermore, the individual might have difficulty getting life insurance or employment when he or she becomes an adult. It is more fair to allow the child to make his or her own decision about testing when he or she becomes an adult at age 18.
The one exception to this childhood testing rule is when it is suspected that the child may have symptoms of juvenile HD. In this case it may make sense to proceed with genetic testing because a positive test would allow for treatment of the symptoms and probably allow the child to have special help in school. In addition, if the test is negative, the family and doctors can eliminate HD as a diagnosis and turn to other possible causes of the symptoms.
It is obviously very hard to care for a child with HD. The most successful approach is to have a well-organized team of parents, teachers, health care providers and others to insure that the child is safe, happy and maturing to the very best of everyone’s ability. In my book the chapter titled “Princess in Pink” describes one such successful support team.
![]()
June 2020 – What Is Late Onset Huntington’s Disease?
The vast majority of persons with HD have the onset of symptoms in middle age, usually between the ages of 30 and 55. However, there is a small, but important group whose onset does not appear until after age 60. This group makes up late onset HD and probably represents 10-15% of the total. There are several things that make this group of special interest.
For example, the late appearance of symptoms is related to the size of the CAG repeat expansion in the HD gene. In late onset the size of this expansion is smaller than in more typical middle age onset. This means that in late onset the CAG size is often in the 37 to 40 range, also known as the reduced penetrance range. Of course these numbers are not exact, but a useful guide. For example in a group of late onset persons we have seen at the University of Washington the CAG repeat expansion size varied from 38 to 44.
This also explains why persons with late onset HD often do not have a positive family history. The CAG expansion size running in their family is relatively small (although still abnormal); thus many people in the family with this size expansion have died of something else (like heart disease) before ever showing symptoms of HD. Two thirds of the late onset persons seen in our Center were the first in their family to be diagnosed with HD.
In the era prior to genetic testing there was an entity called “senile chorea” and no one knew what caused it. With the advent of genetic testing it is now realized that most of this group actually had late onset HD.
It also used to be said that late onset HD was relatively “benign” and not as progressive as earlier onset disease. We now know this is not really accurate. Late onset HD is definitely progressive and the affected persons become more disabled as the years pass. Many eventually require assisted living or a nursing home. Of course elderly persons are also at risk for all the other diseases the can afflict this age group such as heart disease, arthritis, diabetes and cancer. Furthermore, we have seen late onset HD patients who have also developed a more severe progressive dementia. We discovered that, in fact, they had two brain diseases: HD and Alzheimer’s. This is an unfortunate combination, but not too surprising because Alzheimer’s Disease is relatively common.
On the other hand, individuals with late onset HD can be surprisingly hardy. We have seen such persons between ages 88 to 93 still living at home or in assisted living. Their other genes must be especially strong!
Just like all people with HD, but probably even more so, persons with late onset are at high risk for falling and having broken bones or serious head trauma. Gait assistance devices such as walkers are often important additions to their care.
The good news about late onset HD is that these people have had time to have successful careers and family lives prior to the onset of symptoms. In our UW HD Center of Excellence we have seen late onset individuals who have been businessmen and women, military career officers, doctors, lawyers, artists, crafters and scientists. Our communities are better places because of their contributions.
![]()
May 2020 – Huntington’s and COVID-19
 It seems timely and important to say a few words about HD and the COVID-19 pandemic. Unfortunately this virus is lurking everywhere and any person can be a “carrier” without having any symptoms. Certain people are at high risk for having serious consequences of the virus and this includes the elderly and those already affected by another chronic health problem which certainly includes HD. In addition the virus is more common in places where persons have to unavoidably congregate, such as retirement homes, nursing homes, adult care homes, hospitals and prisons. These are all places where persons with HD may be living. We know of two elderly men with HD living in a local retirement homes who had positive COVID-19 virus tests. There are certainly others.
It seems timely and important to say a few words about HD and the COVID-19 pandemic. Unfortunately this virus is lurking everywhere and any person can be a “carrier” without having any symptoms. Certain people are at high risk for having serious consequences of the virus and this includes the elderly and those already affected by another chronic health problem which certainly includes HD. In addition the virus is more common in places where persons have to unavoidably congregate, such as retirement homes, nursing homes, adult care homes, hospitals and prisons. These are all places where persons with HD may be living. We know of two elderly men with HD living in a local retirement homes who had positive COVID-19 virus tests. There are certainly others.
A very recent medical report from Italy and London found that elderly patients with Parkinson’s disease were more likely to have serious cases of COVID-19 infection and had a high mortality rate (40-50%). Parkinson’s is a chronic degenerative neurologic disease just like HD, so these findings may be similar to those to be expected with HD.
So what can be done? First is to be aware of COVID-19 symptoms. These usually are cough, sore throat, muscle aches, trouble breathing, fever, headache and new loss of taste or sense of smell. Older persons may especially have fatigue, loss of energy, confusion and decreased appetite. These symptoms should immediately be brought to the attention of care givers and such persons should be tested for the virus. The other important strategy is to be proactive to prevent getting or spreading the virus. These actions are frequent hand washing, wearing a face mask when out in public and practicing social distancing. Washingtonians seem to have mostly taken these messages to heart and our state is doing relatively well in these difficult and trying times.
Finally, stay in touch with family and friends (at a distance of course): social interaction helps prevent depression. We will make it through this together.
Stay safe and stay healthy!
![]()