Last week, Dr. Thomas Grabowski, Director of the UW Memory and Brain Wellness Center and the UW Alzheimer's Disease Research Center (ADRC) flew across the country to serve as a witness on a Senate Appropriations Subcommittee hearing, 'Saving Lives for Medical Research.' He, along with three other medical experts in cancer and infectious diseases, had the opportunity to help the senators in their mission of establishing priorities and guiding the administration in making decisions about National Institutes of Health (NIH) funding appropriations in the federal budget. [Full Video]
The National Institute on Aging, within the NIH, funds the 32 ADRCs across the country. "NIH funding is what gives longevity to the research infrastructure, brings about standardization and thematic direction, enables cooperation at scale, and trains new scientists," Dr. Grabowski stated in his opening statement (PDF). "We need to bring about even more cooperation across NIH, industry, and charitable groups; and new standards of data sharing to promote progress."
In December, Democrats and Republicans agreed on a new $4.8 billion funding stream for the NIH in the 21st Century CURES Act to help accelerate medical research efforts, $1.6 billion of which will go to research on brain diseases. In terms of Alzheimer's disease specifically, NIH Director Francis Collins recently analyzed the funding needed in 2018 to remain on track to achieve the goals of the National Plan to Address Alzheimer’s Disease to prevent and effectively treat Alzheimer’s disease by 2025.
Collins has recommended an additional $414 million increase in spending above NIH’s base appropriation, through a NIH Professional Judgment Budget. That increase would bring overall NIH Alzheimer’s research funding to $1.8 billion per year, quadruple what it was a few years ago. To date, only cancer and HIV/AIDS have received one of these special budgets, which bypass the traditional Federal budget modification process and go straight to the Executive Branch and Congress. (Congress has yet to approve the NIH's 2017 professional judgment budget for Alzheimer's research.)
"I urge it on you with enthusiasm, and with optimism that we can defeat this disease," stated Dr. Grabowski.
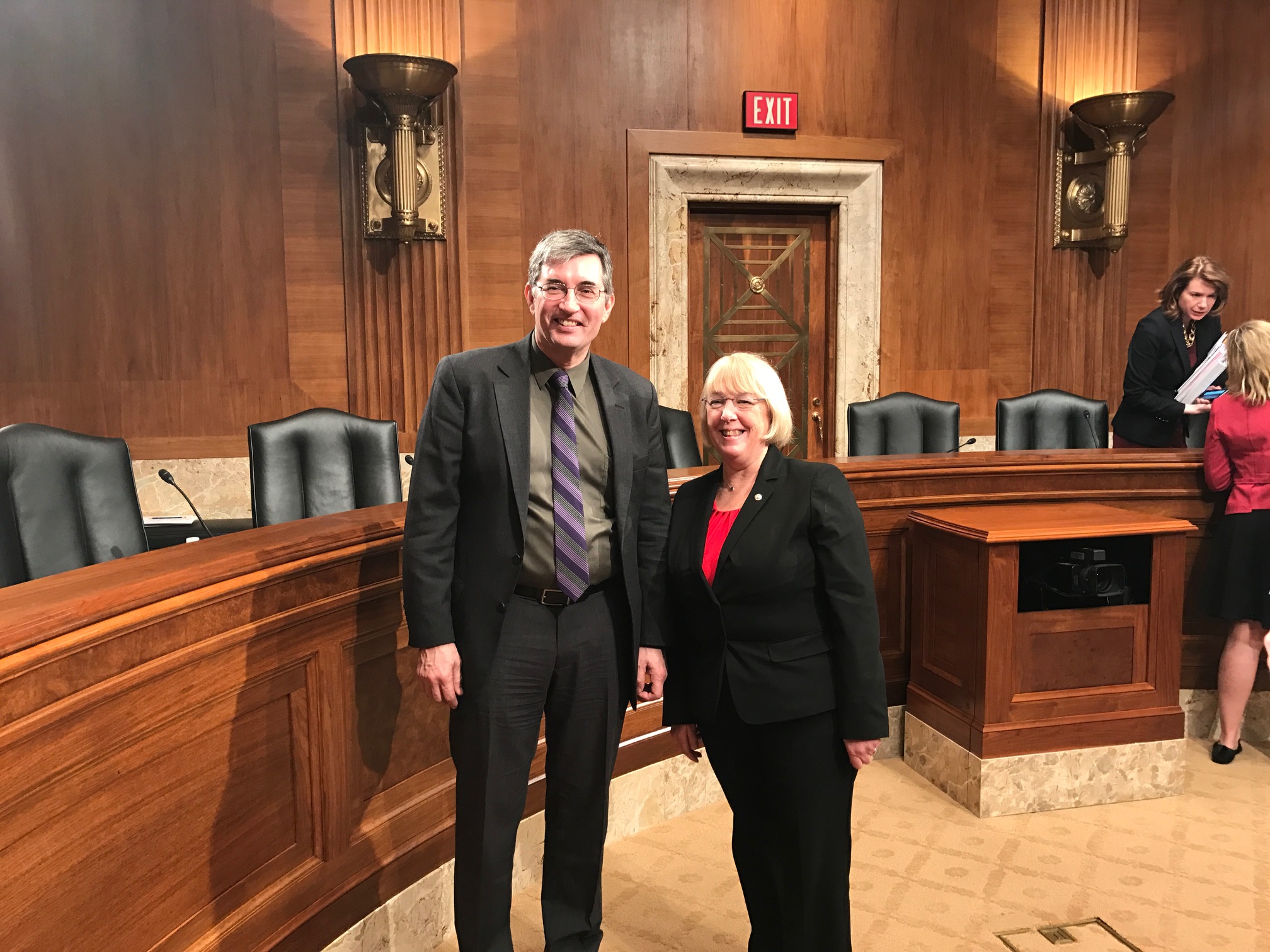
The senators peppered the experts with questions. Patty Murray (D-WA) asked Dr. Grabowski about the research aims and challenges at the UW ADRC. "Why are you hopeful this approach will speed the search for treatments?" and "What are the biggest barriers to finding an effective treatment for Alzheimer's disease?"
He explained that Alzheimer's is not just one disease. The pathological processes that lead to memory loss and dementia are incredibly heterogeneous across people. Effective treatment will require targeting the biological pathways that drive disease in individual people, an approach called precision medicine. "The field has focused heavily on amyloid protein processing and has launched clinical trials for people at risk of amyloid-driven Alzheimer's disease," he said, "but we also have to understand other pathways, such as immune response and protein trafficking, to treat others."
Acknowledging the hills still to climb, Dr. Grabowksi said that researchers don't entirely understand why amyloid and tau proteins become toxic to brain cells. Researchers also want to know how education and lifestyle factors endow resistance to dementia, on a biological level. "We have relied on studying these mechanisms in transgenic mouse models of Alzheimer's disease, but they haven’t yielded effective treatments in humans. We need to pursue more human relevant models, such as the promising patient-derived stem cell research at the UW ADRC," he said, referring to the work of ADRC’s Drs. Jessica Young and Dirk Keene. "That's the point of the Professional Judgment Budget Funding Year 2018."
Dick Durbin (D-IL) asked if researchers can tell if someone will develop the disease before they show symptoms, and why this is valuable.
"Biomarker and amyloid imaging technologies have advanced to the point that amyloid build-up can be detected in brain years ahead of time," Dr. Grabowski said. "Fully 20% of people age 65 and older will have a positive amyloid scan, signaling latent disease, so there's a long period of time when we could provide interventions to slow or prevent the symptoms."
Presiding member chairman Roy Blunt (R-Missouri) inquired about the possibility of reducing the future costs of dementia to the health care system and families.
"By 2050, cases of Alzheimer's disease will about triple, so were talking a trillion dollars of direct and opportunity costs," said Grabowski. "The incidence of Alzheimer's disease-type dementia doubles every 5 years after age 65, and so if we could delay onset by 5 years, we could cut the number of cases in half, and by inference, we could cut dementia-related costs in half."
The senators thanked the panel of experts for their time and emphasized their ultimate goal to fund NIH medical research at increasing levels each year. But first, they must work together to prioritize NIH funding during the imminent budget decisions.
Now back in Seattle, Dr. Grabowski has had time to reflect on the experience. "I came away from the hearing realizing that the bipartisan subcommittee members really seem interested in marshalling material to support the continuing robust funding of the NIH, but it also sounded like the recent budget proposals for increased Alzheimer's disease research funding remain on uncertain ground." —Genevieve Wanucha
Photos credit Alex Keenan