By Genevieve Wanucha
As published in Dimensions Magazine - Fall 2018
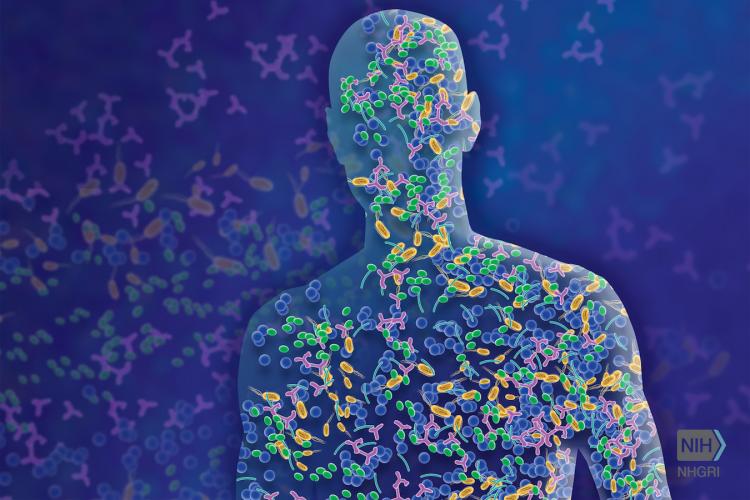
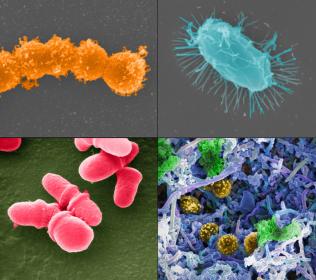
Bacteroides, Bifidobacteirum, Faecalibacterium, Ruminococcus– these are the names of some of the 100 trillion bacteria who are living and working in your gut. These microscopic critters, collectively known as the microbiome, help our body to digest food, process nutrients, make vitamins B and K, and produce immune molecules that fight inflammation and heal wounds. The most impressive role of this busy workforce may be, surprisingly, in the brain.
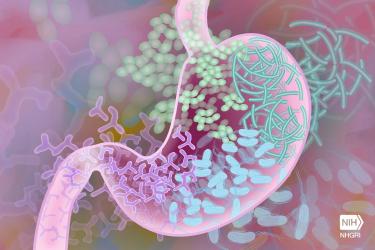
While the digestive tract and the brain feel far apart in your body, they are actually connected via a 24/7 direct line of biochemical communication, set up by special nerve cells and immune pathways. It’s called the gut-brain axis. Down in the gut, bacteria make neuroactive compounds, including 90% of our neurotransmitter serotonin, which regulate our emotions. In turn, the brain can send signals to the gastrointestinal system, for example, to stimulate or suppress digestion.
A healthy microbiome is a diverse microbiome. A rich community of varied species protects against one dominating and causing trouble in our gut and beyond. Shifts in the composition or function of the microbiome have been implicated in inflammatory bowel disease, autism, and blood cancers. Researchers are now discovering that a disrupted microbiome, in certain contexts, may contribute to Alzheimer’s disease and related conditions that cause dementia.
“The role of the microbiome in health and disease is an exciting area at the forefront of science, but the field is in its infancy,” says Dr. William Depaolo, a UW Medicine gastroenterologist and director of the UW Center for Microbiome Sciences & Therapeutics. “I think about the microbiome like a biologist thinks about the deep sea. We know there’s something down there, and we finally have the technology to help us see who’s actually there and how they are influencing our bodies and brains.”
Advanced tools of ‘multi-omics’ technology allow researchers to identify species in the human gut and analyze the bacterial genes and protein products that affect our brain health. Recently, NIH-funded research conducted at the Wisconsin Alzheimer’s Disease Research Center examined the microbiomes of people with Alzheimer’s disease. The team, led by Barbara Bendlin, PhD, and Frederico Rey, PhD, collected stool samples from participants and used genetic sequencing technology to identify the bacterial species present, and assess the microbial richness and diversity.
They found that people living with Alzheimer’s disease have a unique, and less diverse, community of gut microorganisms than their healthy counterparts. Specifically, the microbiomes of people with Alzheimer’s disease showed specific increases and decreases in common gut bacteria, especially decreases in Bifidobacterium, an important inhabitant of the healthy human gut. They also linked the abnormal levels of these microbe families to the amount of Alzheimer’s disease proteins in the participants’ spinal fluid.
The authors suggest that the unique microbiome of people with Alzheimer’s disease could be contributing to the progression of their disease, through the gut-brain axis. Such findings in human and mouse models point to the tantalizing prospect that restoring healthy gut bacterial composition could prevent or slow the development of Alzheimer’s in at-risk populations.
The microbiome field is optimistic about this therapeutic approach. “We know that diet can profoundly affect the microbiome,” says Dr. Depaolo, whose UW lab studies the influence of the microbiome on health and many diseases.“We know that bacterial cells are more sensitive to drugs than human cells, so we can target them without hitting human cells. So, there is a lot of excitement here in using multi-omics technology to identify microorganisms that we could promote in specific people or find strategies to manipulate the microbiome.”
But, as with all quests to create precise, targeted therapeutics for Alzheimer’s disease, it all comes down to genetics.
It’s in the Genes
The composition of every person’s microbiome is unique as a fingerprint, shaped by early life, diet, and environmental exposures over time. But it is our genetic background that influences how bacteria actually function in the human gut. What’s more, bacteria themselves express different genes and make proteins that may predispose certain individuals to gut inflammation or other conditions.
In one striking example, recent NIH-funded research conducted by researchers in the NeuroGenetics Research Consortium suggested that Corynebacterium helps cause Parkinson’s disease, but only in people with a specific genotype.
The study focused on the gene SNCA rs356219, a known genetic risk factor for Parkinson’s disease. However, it’s not strong enough to cause the disease by itself. Scientists have long suspected a trigger. In the study led by Dr. Zachary Wallen, PhD, and Dr. Haydeh Payami, PhD, of the University of Alabama, researchers took blood samples from 197 middle-aged patients with Parkinson’s disease and 115 age-matched controls and determined the “genotype,” or version, of SNCA rs356219. (Human beings have one of three genotypes of SNCA rs356219: AA, GA, or GG.)
They also extracted DNA from stool samples to see what bacteria were in their guts and then looked for interactions between the SNCA rs356219 genotype, gut microbiome, and Parkinson’s disease risk.
The team found that Corynebacterium was most abundant in people with the GG genotype. Every person who had the GG genotype and Corynebacterium in the gut also had Parkinson’s disease. Could there be something about the GG genotype that affects or jumpstarts this bacterium’s production of disease proteins in the gut?, the researchers ask.
Corynebacterium is a common bacterium on human skin, and researchers don’t know how enters it the gut, why some people have more than others, or if it could be a target for an antibiotic. The findings were presented at the 142nd Annual Meeting of the American Neurological Association.
While this study needs to be replicated in a larger population, the findings show how important it will be to consider a patient’s genetic factors in microbiome research. “The issue of genetic influence cannot be ignored in this field,” says Dr. Depaolo. “We don’t yet know how genetics influence the microbiome, or how genes in bacteria are regulated. Before we start giving bacteria, antibiotics, or fecal transplants to people, we need to address the very basic question of how different genetic backgrounds affect the microbiome.”
How About Probiotics?
While we can’t change our genes, we can modify our exposures and diet to nurture our microbiome as we age. General consensus holds that consuming fermented foods have some benefit to gut health, especially for those on anti-biotic medications. These are foods full of healthy ‘probiotic’ bacteria, such as yogurt, kefir, kombucha, sauerkraut, and kimchi. Common foods that feed the healthy gut bacteria include garlic, onions, Jerusalem artichoke, leeks, asparagus, bananas, barley, oats, apples, cocoa, wheat bran, burdock root, and flaxseeds, to name a few.

Common foods that feed the healthy gut bacteria include garlic, onions, Jerusalem artichoke, leeks, asparagus, bananas, barley, oats, apples, cocoa, wheat bran, burdock root, and flaxseeds.
“To get your microbiome into the best composition you can, I think it’s reasonable to make sure to get enough fiber in your diet,” says Dr. Angela Hanson, MD, research scientist and geriatrician at UW Memory and Brain Wellness Center. “Consider eating yogurt with active cultures and talking to your doctor about probiotic supplements if you need to be on antibiotics for an infection.”
There’s a whole list of questions to answer before diet advice can get more specific than yogurt and kale: How does diet impact the microbiome long-term? How long does it take to permanently alter the gut microbiome? Can friendly bacteria in fermented foods actually establish long-lasting colonies in the gut? There has been a lack of human studies on the long-term health effects of fermented foods or probiotic supplements, which do not have FDA approval.
That said, consuming healthy bacteria has real health effects. “Probiotics do stimulate immune and epithelial cells and produce anti-inflammatory short-chain fatty acids in the intestines, which can help keep gut inflammation from getting out of control,” says Dr. Depaolo. “But, taking just any probiotic won’t replace a community of Lactobacillus after you’ve lost it. You would have to take a probiotic suited to you.”
Individualized probiotics don’t yet exist, but the microbiome is beginning to enter into Alzheimer’s disease research, mainly through the NIH-funded Alzheimer's Disease Metabolomics Consortium. Additionally, NIH Alzheimer’s Disease Research Centers around the country are collecting microbiome samples of study participants, in support of efforts to finally map the microbiome gut-brain communication axis in people with Alzheimer’s disease.
For now, let’s keep in mind that our microbiome has kept us alive all of these years – and that team of 100 trillion will need a little more help as it gets older.